Nebula Genomics DNA Report for Emphysema
Is emphysema genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

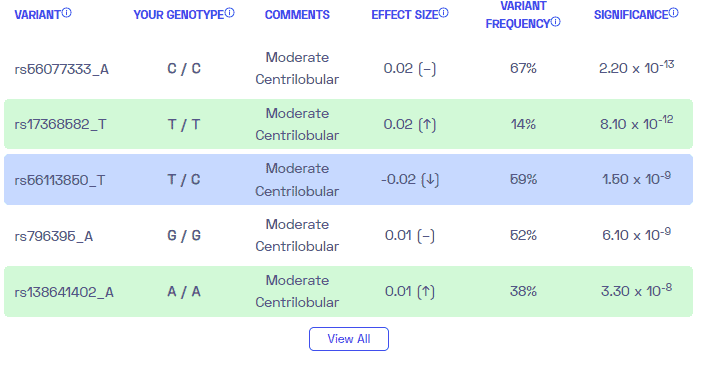
Table of contents
What is Emphysema?
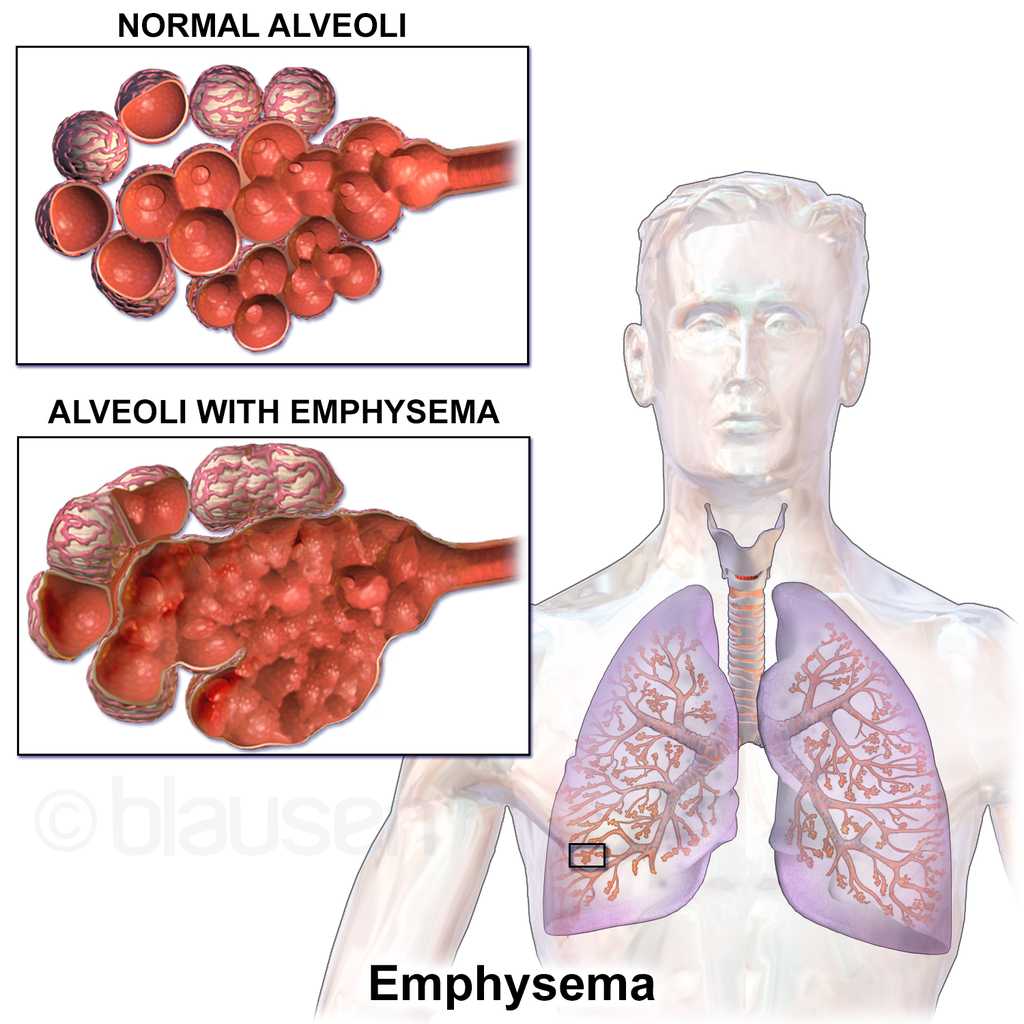
Emphysema, a type of COPD (chronic obstructive pulmonary disease), characterized by the irreversible destruction of the air sacs in the lungs. The larger surface area reduces the amount of gas exchange, resulting in damaged lungs that cause breathing difficulties.
This progressive lung condition damages the walls of the air sacs (alveoli), causing them to lose their elasticity, and eventually rupture. This leads to reduced lung function and impaired ability to exhale properly.
The condition is primarily caused by long-term exposure to irritants, with cigarette smoke being the most common culprit. Other factors, such as occupational exposure to dust and chemicals, air pollution, and secondhand smoke, can also contribute to the development of emphysema.
Is Emphysema Genetic?
While experts believe environmental factors predominantly cause emphysema, there is evidence to suggest that genetic factors play a role in an individual’s susceptibility to the disease.
Some of the genetic factors involved are:
- SERPINA1 Gene: The SERPINA1 gene provides instructions for producing the alpha-1 antitrypsin protein. Mutations in this gene can cause alpha-1 antitrypsin deficiency, an inherited disorder that causes lung and liver disease. The alpha-1 antitrypsin protein helps protect the lungs from the destructive effects of enzymes called proteases. Individuals with AATD have an increased susceptibility to lung damage and emphysema, particularly in those who smoke. About 15% also develop liver damage (cirrhosis).
- SFTPC (Surfactant Protein C): Surfactant proteins play a crucial role in maintaining the elasticity and integrity of the alveoli in the lungs. Mutations in the SFTPC gene, which codes for surfactant protein C, have been identified in individuals with familial interstitial lung disease and emphysema. These mutations can disrupt lung function.
- TERC (Telomerase RNA Component): Telomeres are protective caps at the ends of chromosomes that shorten with each cell division. The TERC gene encodes a component of the enzyme telomerase, which helps maintain telomere length. Mutations in the TERC gene can lead to telomere shortening and impaired lung cell regeneration.
- MMP12 (Matrix Metalloproteinase 12): Matrix metalloproteinases (MMPs) are enzymes involved in tissue remodeling and inflammation. Increased expression of MMP12, encoded by the MMP12 gene, has been observed in emphysema patients. MMP12 plays a role in the destruction of lung tissue.
- GSTM1 (Glutathione S-transferase M1): Glutathione S-transferases (GSTs) are enzymes involved in detoxification processes, including the neutralization of harmful substances. The GSTM1 gene encodes an isoform of GST. Variations in the GSTM1 gene, specifically the GSTM1 null genotype, have been associated with an increased risk of developing emphysema, particularly in individuals exposed to cigarette smoke.
Epidemiology
Emphysema, as a part of COPD, has a significant global impact on public health. According to the World Health Organization (WHO), COPD prevalence was around 251 million cases worldwide in 2016. Experts estimate that approximately 90% of COPD-related deaths occur in low and middle-income countries. In 2019, COPD ranked as the third leading cause of death globally, accounting for 3.23 million deaths.
In the United States, the prevalence of emphysema is approximately 14 million cases. This includes 14% of white male smokers and 3% of white male nonsmokers. The prevalence is slightly lower for white female smokers and African Americans. These specific patient groups tend to develop emphysema with less exposure time compared to other populations.
The incidence of emphysema is slowly increasing, primarily due to the rise in cigarette smoking rates and environmental pollution. Additionally, improvements in mortality rates from other causes, such as cardiovascular diseases and infectious diseases, have contributed to a larger proportion of the population reaching older ages and being at higher risk for developing the condition.
Symptoms
Recognizing the symptoms of emphysema is crucial for early detection, prompt diagnosis, and appropriate management. Unfortunately, the signs of the condition can be subtle. The main system is shortness of breath, which occurs gradually.
It usually starts during activity. As the disease progresses, patients may start to notice they become out of breath while at rest.
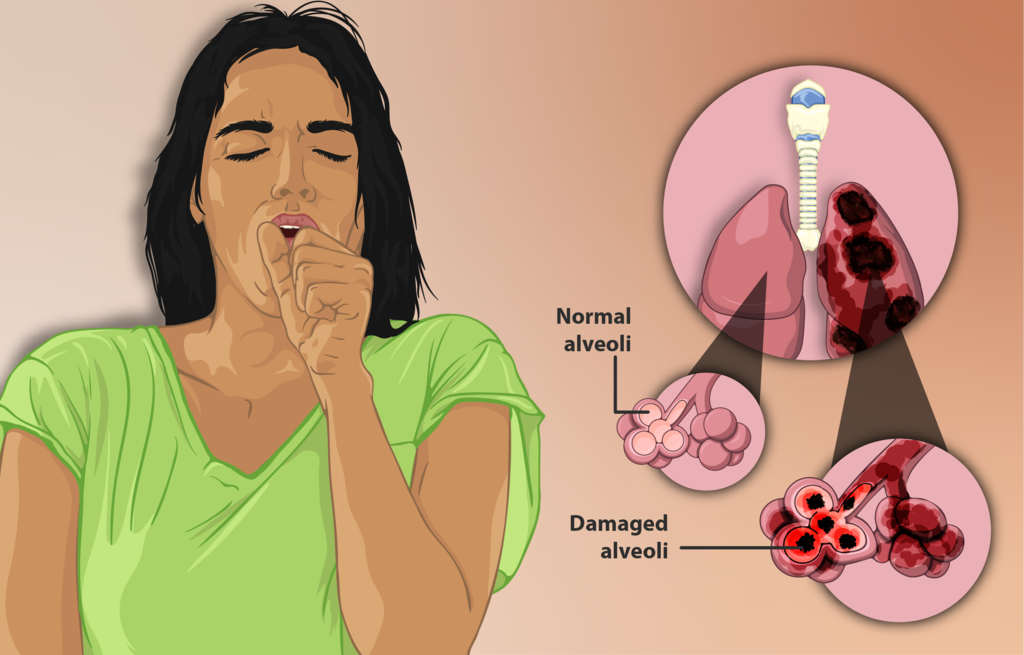
People with emphysema may also experience a persistent cough, wheezing, fatigue, weight loss, and chest tightness. Sometimes, they get frequent respiratory infections such as colds and flus.
Causes
Emphysema is caused by a combination of genetic factors and prolonged exposure to environmental irritants.
The main airborn irritants contributing to emphysema are tobacco smoke, marijuana, air pollution, and chemical fumes or dust.
Non-smokers may also develop emphysema, indicating the role of genetic factors and individual susceptibility in the disease’s development.
Diagnosis
The diagnosis of emphysema involves a thorough assessment of the patient’s medical history, a physical examination, and the use of specialized tests. The doctor may rule out similar conditions. For example, emphysema and chronic bronchitis present similar symptoms, but the latter is reversible.
Pulmonary function tests, especially spirometry, are crucial for diagnosing and evaluating the severity of emphysema. This test uses an instrument the patient blows into, called a spirometer. It measures the volume and flow of air inhaled and exhaled by the lungs. It also assesses lung capacity, airflow limitations, and the presence of obstruction.
A doctor may also measure arterial blood gas to determine the stage of the condition.
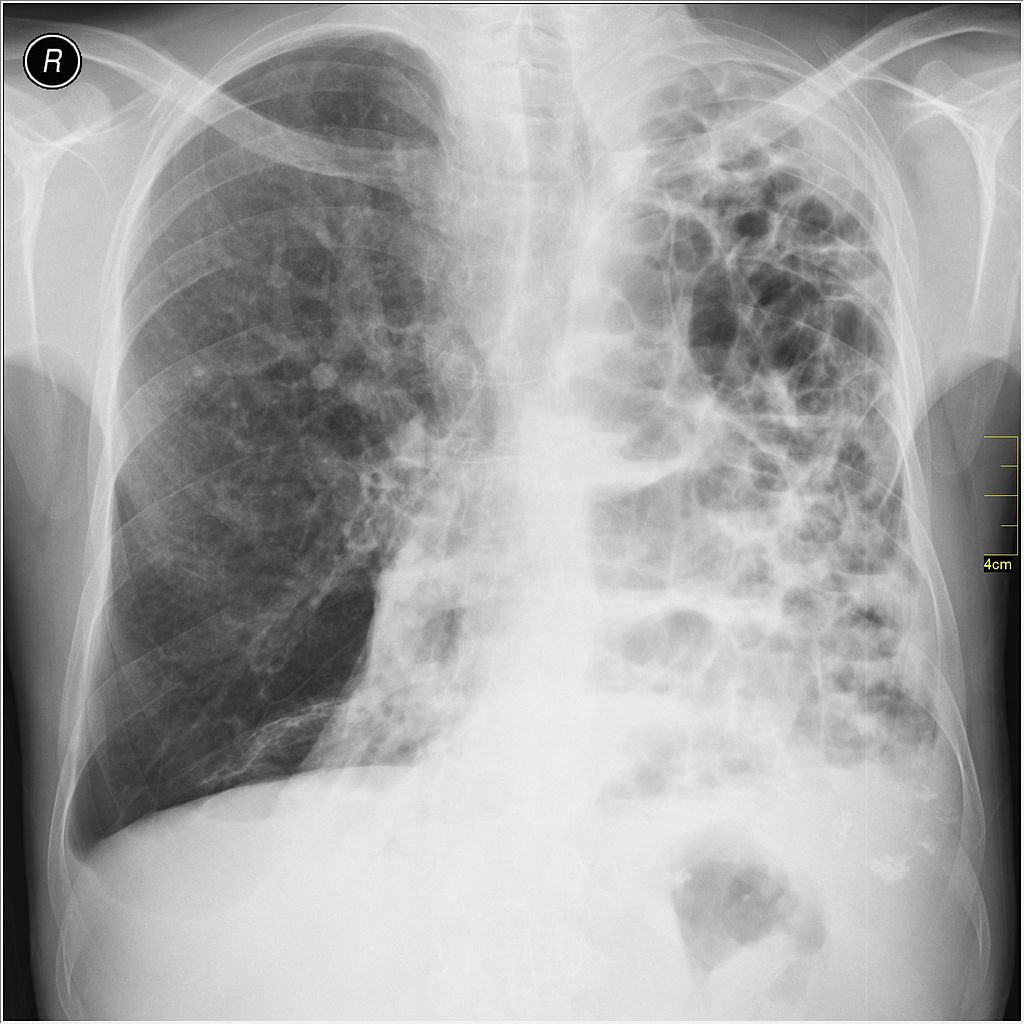
Chest x-rays can reveal hyperinflation (increased lung size), flattened diaphragms, and decreased lung markings, which may suggest emphysema. However, chest X-rays alone may not be sufficient for an accurate diagnosis, as early-stage emphysema may not show noticeable abnormalities. Therefore, doctors may use a CT scan, which takes images from multiple directions to get a more useful image.
Doctors may also recommend a blood test to determine how well the lungs transfer oxygen into, and remove carbon dioxide from, the bloodstream.
In certain cases, genetic testing may be recommended, particularly if alpha-1 antitrypsin deficiency (AATD) is suspected. Genetic testing helps identify specific mutations in the SERPINA1 gene associated with AATD. It also aids in identifying family members who may be at risk.
Treatment
There is no cure for emphysema or COPD. Instead, the management of emphysema aims to alleviate symptoms, slow disease progression, and improve quality of life.
Quitting smoking and avoiding environmental irritants, such as secondhand smoke and air pollutants, are crucial steps in managing emphysema. These measures help prevent further lung damage and improve overall respiratory health.
A doctor may recommend several therapy options. Pulmonary rehabilitation programs combine exercise training, breathing techniques, and education to improve lung function. These programs are tailored to individual needs and can significantly improve quality of life. Nutrition programs can also help patients manage symptoms, especially for those who need to lose or gain weight.
In advanced cases of emphysema when oxygen levels in the blood are low, supplemental oxygen therapy may be necessary. Patients use oxygen at home with a machine that delivers it directly through the nostrils. Some may only need supplemental oxygen when they exercise while others may use it continuously. Oxygen therapy helps improve oxygenation, relieve breathlessness, and enhance exercise capacity.
Medications prescribed for emphysema include bronchodilators, which help relax the airway muscles and improve breathing. Doctors may also recommend inhaled corticosteroids, which reduce lung inflammation. These medications provide symptomatic relief, reduce exacerbations, and improve lung function.
For some individuals with severe emphysema, surgical interventions may be considered. Lung volume reduction surgery involves removing damaged portions of the lung. With the damaged portions removed, the remaining lungs can act more efficiently to improve lung function and breathing. Alternatively, lung transplantation is an option for individuals with end-stage emphysema for whom other options have failed.
If you liked this article, you should check out our other posts in the Nebula Research Library!
August 3, 2023