Informe de ADN de Nebula Genomics para la esquizofrenia
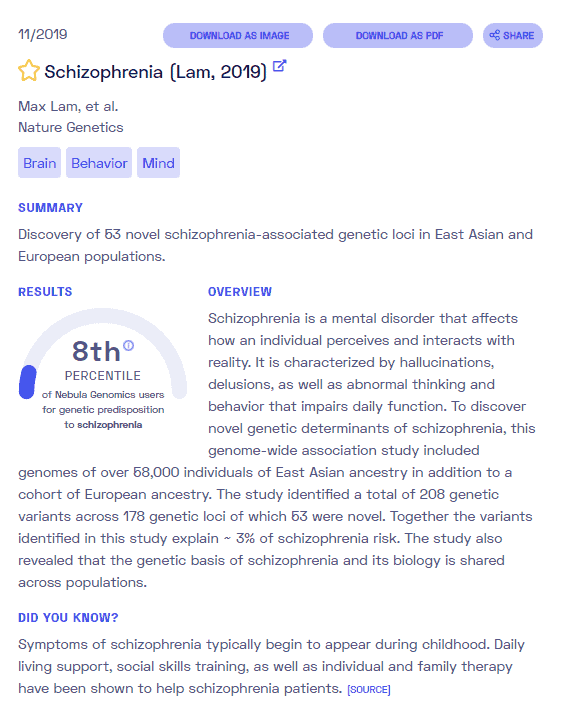
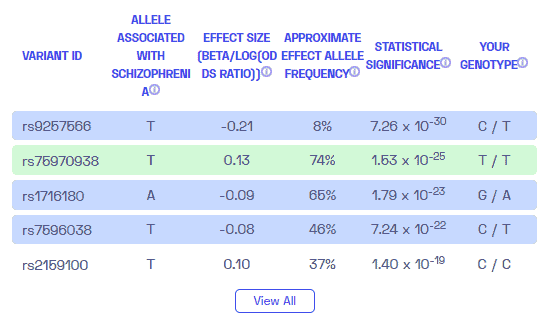
¿La esquizofrenia es genética? Creamos un informe de ADN basado en un estudio que intentó responder esta pregunta. A continuación puede ver un informe de MUESTRA de ADN. Para obtener su informe de ADN personalizado, compre nuestro Secuenciación del genoma completo !
Información Adicional
¿Qué es la esquizofrenia? (Parte 1 de ¿La esquizofrenia es genética?)
El término esquizofrenia se refiere a una enfermedad mental grave o trastorno psicótico con síntomas similares al de las psicosis, donde el paciente interpreta la realidad de forma anormal.
En la etapa aguda de la enfermedad, una persona esquizofrénica padece una variedad de trastornos característicos que afectan casi todas las áreas de la experiencia y el comportamiento. Esto incluye percepción, pensamiento, vida emocional y emocional, formación de la voluntad, habilidades psicomotoras e impulso.
A menudo, los pacientes escuchan voces que realmente no están presentes. Además, puede ocurrir la ilusión de ser seguido, espiado o controlado. También son posibles las alucinaciones persistentes de cualquier modalidad sensorial.
Una persona con esquizofrenia a menudo mostrará características que aparecen como aislamiento social, falta de impulso, falta de motivación, aplanamiento emocional y falta de alegría. Dependiendo de los síntomas predominantes, se distinguen varios subgrupos de esquizofrenia. Es importante tener en cuenta que la esquizofrenia y el trastorno de personalidad dividida no son lo mismo. El primero no se asocia con múltiples personalidades como lo hace el segundo. La esquizofrenia también es distinta de trastorno bipolar , una enfermedad mental diferente que provoca cambios extremos de humor.
En muchos casos, los síntomas desaparecen después de la fase inicial de la enfermedad. A partir de entonces, pueden seguir fases posteriores de recaídas de la enfermedad o episodios de psicosis a intervalos irregulares. En aproximadamente un tercio de los pacientes, todos los síntomas desaparecen por completo después de cierto punto. En aproximadamente otro tercio, las recurrencias ocurren repetidamente. En el último tercio, el curso de la enfermedad se vuelve crónico y conduce a una discapacidad mental permanente.
Epidemiología (Parte 2 de ¿La esquizofrenia es genética?)
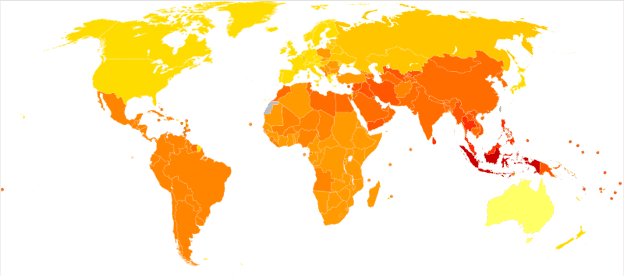
A partir de 2019, se sabe que la esquizofrenia afecta a 20 millones de personas en todo el mundo. No es tan común como otras condiciones de salud mental. Las personas que desarrollan la afección tienen entre 2 y 3 veces más probabilidades de morir antes que la población general debido a enfermedades físicas, como enfermedades cardiovasculares, metabólicas e infecciosas.
El riesgo de desarrollar la enfermedad es el mismo para hombres y mujeres, aunque generalmente la esquizofrenia afecta a los hombres a una edad un poco más temprana. Los hombres pueden presentar síntomas entre principios y mediados de los 20, mientras que los síntomas de una mujer suelen comenzar a finales de los 20. Es poco común que los niños sean diagnosticados con esquizofrenia y poco común para los mayores de 45 años.
Síntomas (Parte 3 de ¿La esquizofrenia es genética?)
Los síntomas de la esquizofrenia se dividen tradicionalmente en dos grandes áreas: síntomas positivos y síntomas negativos. Recientemente, los síntomas cognitivos del trastorno también han recibido una atención cada vez mayor y se consideran una tercera área separada.
De acuerdo a Mayo Clinic Los signos y síntomas pueden variar entre individuos, pero generalmente incluyen delirios, alucinaciones o habla desorganizada, y reflejan una capacidad de funcionamiento deteriorada. El pensamiento puede convertirse en un paso corto y las relaciones de múltiples capas ya no pueden entenderse en su complejidad. La expresión lingüística se empobrece.
La gravedad de los síntomas depende en parte de la personalidad de la persona afectada. Aunque los síntomas varían mucho entre individuos, los pacientes individuales a menudo conservan su patrón individual de síntomas durante largos períodos de tiempo. Una vez que a una persona se le diagnostica esquizofrenia, puede explorar opciones de tratamiento como la prescripción de medicamentos antipsicóticos o asistir a grupos de apoyo. Los pacientes serán monitoreados constantemente para detectar recaídas y efectos secundarios a largo plazo.
Síntomas positivos
Los síntomas positivos se refieren a exageraciones de la experiencia normal y, por tanto, se ven como una especie de «exceso» del estado de salud. Estos incluyen conceptos erróneos graves de la realidad experimentada, como alucinaciones y pérdida de la realidad. La esquizofrenia con síntomas predominantemente positivos a menudo comienza repentinamente y, a menudo, no hay características visibles antes del inicio de la afección. El curso de la enfermedad es bastante favorable.
Hay varios síntomas positivos de la esquizofrenia que incluyen:
- Alucinaciones. Creencias falsas que no se basan en la realidad. Por ejemplo, piensa que está siendo lastimado o acosado; otra persona está enamorada de ti; o una gran catástrofe está a punto de ocurrir. Los delirios son uno de los síntomas más comunes en las personas con esquizofrenia.
- Alucinaciones. Ver u oír cosas que no existen. Si bien las alucinaciones pueden darse en cualquiera de los cinco sentidos, escuchar voces es la alucinación más común.
- Pensamiento desorganizado (habla). El pensamiento desorganizado se observa cuando el habla se vuelve desorganizada. La comunicación eficaz puede verse afectada y las respuestas a las preguntas pueden no tener relación parcial o total.
- Comportamiento motor extremadamente desorganizado o anormal. Estos síntomas varían desde tonterías infantiles hasta agitación impredecible. Es difícil para las personas realizar tareas. El comportamiento puede incluir resistencia a las instrucciones, una postura inapropiada o extraña, una falta total de respuesta o un movimiento inútil y excesivo.
Síntomas negativos
Los síntomas negativos se refieren a limitaciones en la experiencia normal y las funciones mentales que estaban presentes anteriormente pero que se han reducido o ausente por completo debido a la enfermedad. Por tanto, estos síntomas representan una deficiencia en comparación con el estado de salud.
Por ejemplo, la persona puede descuidar la higiene personal o parecer carente de emociones (no hace contacto visual, no cambia las expresiones faciales o habla en un tono monótono). La persona puede perder interés en las actividades cotidianas, retraerse socialmente o carecer de la capacidad de experimentar placer.
La esquizofrenia con síntomas negativos pronunciados a menudo comienza gradualmente y el curso de la enfermedad puede ser desfavorable. Los síntomas negativos pueden ocurrir meses o años antes de los síntomas psicóticos agudos. Los primeros síntomas suelen ser trastornos del sueño y síntomas depresivos. Los síntomas negativos suelen intensificarse o endurecerse con el aumento de la duración de la enfermedad.
Causas (Parte 4 de ¿La esquizofrenia es genética?)
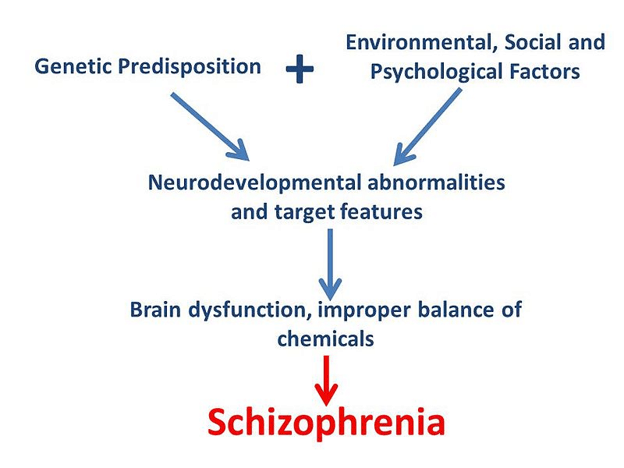
No se ha identificado una sola causa de esquizofrenia. A partir de 2020, se supone que existe una interacción de varios factores desencadenantes
La explicación general de la causa de la esquizofrenia se basa actualmente en una interacción multifactorial de causas biológicas (por ejemplo, genéticas, infecciosas, metabólicas) y psicosociales (por ejemplo, entorno social, estrés psicológico en la biografía). En consecuencia, varios de estos factores combinados pueden desencadenar la esquizofrenia. Exceder un umbral de estrés se considera el factor desencadenante que hace que la psicosis estalle en una persona biológicamente susceptible (vulnerable).
¿La esquizofrenia es genética?
La investigación sugiere que los genes juegan un papel en el factor de riesgo de desarrollar esquizofrenia. Sin embargo, no existe un único «gen de la esquizofrenia». Un pequeño porcentaje de pacientes con esquizofrenia parece tener una pequeña deleción (microdeleción) en una región de cromosoma 22 , conocido como 22q11. Como tal, generalmente se considera que una combinación de factores genéticos y ambientales conduce a la esquizofrenia.
Se sabe que tener un miembro de la familia con o antecedentes familiares de esquizofrenia aumenta el riesgo de desarrollar el trastorno. En el caso de un padre esquizofrénico, es de cinco a diez por ciento de probabilidad de que un niño lo desarrolle. En el caso de los hermanos, es del ocho al diez por ciento. En el caso de los gemelos idénticos, el 45 por ciento y alrededor del 21 por ciento en el caso de los gemelos fraternos.
Sin embargo, en el contexto de la interacción gen-ambiente, por ejemplo, las complicaciones del nacimiento como la falta de oxígeno, la infección o el estrés de la madre, aumentan el riesgo de desarrollar esquizofrenia. Los pacientes con esquizofrenia tienden a tener defectos del sistema inmunológico. Los factores biográficos, psicológicos y sociales también pueden ser significativamente responsables del desarrollo de la esquizofrenia si existe vulnerabilidad genética.
Factores no genéticos
Neurobiología
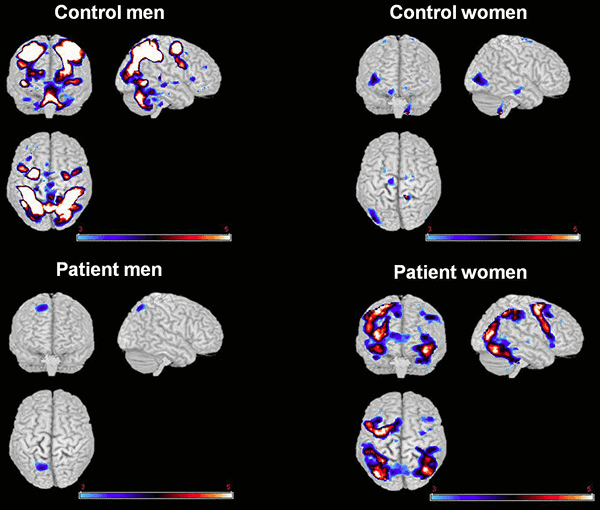
Las técnicas de imagen demuestran que el cerebro muestra múltiples variaciones en anatomía y fisiología en casos de esquizofrenia. Una investigación reciente busca aclarar la conexión entre ciertas desviaciones y el curso esperado de la enfermedad.
El diagnóstico de esquizofrenia también se acompaña de cambios bioquímicos en el cerebro. Por ejemplo, el transmisión de señal entre las células nerviosas del cerebro se desvía de su funcionamiento normal con respecto a los sistemas de neurotransmisores que trabajan con dopamina, GABA o glutamato.
La esquizofrenia también parece desarrollarse cuando hay un desequilibrio de un neurotransmisor llamado dopamina, y posiblemente también serotonina, en el cerebro.
Factores tóxicos
En general, el uso de sustancias que alteran fuertemente la conciencia conduce a un mayor riesgo de esquizofrenia. Sin embargo, también depende tanto de la disposición genética como de la personalidad individual. Psicotrópico sustancias como el alcohol, las anfetaminas, la cocaína y la fenciclidina pueden desencadenar psicosis inducidas por sustancias.
También se sabe que las sustancias que no alteran la conciencia, como los esteroides, pueden causar psicosis.
Factores hormonales
Ha habido evidencia durante muchas décadas de que los estrógenos influyen en el riesgo de la enfermedad y la gravedad de los síntomas. Más recientemente, se ha demostrado que, como complemento al tratamiento farmacológico normal, los moduladores selectivos del receptor de estrógeno, como raloxifeno , puede reducir levemente los síntomas de la esquizofrenia y puede usarse durante períodos de tiempo más prolongados, tanto en mujeres como en hombres.
Factores psicosociales
Los déficits del desarrollo del ego o el abandono grave en los primeros años de vida pueden ser factores que conduzcan a una mayor susceptibilidad a las enfermedades, aumentando la vulnerabilidad. El trauma durante el nacimiento, la desnutrición antes del nacimiento, las infecciones virales y el trauma adicional también pueden contribuir al desarrollo de la enfermedad.
En un amplio Estudio de seguimiento , se encontró que los hijos de madres que habían descrito a su hijo como «no deseado» al final del embarazo tenían más del doble de probabilidades de desarrollar esquizofrenia durante su vida como grupo de control. Según los autores, los resultados sugirieron que el estrés psicosocial durante el embarazo o una tendencia particular en el comportamiento general de la madre estaba asociado con un mayor riesgo.
También hay evidencia de que la incidencia de trauma infantil en las biografías de personas con esquizofrenia aumenta estadísticamente.
Diagnóstico (Parte 5 de ¿La esquizofrenia es genética?)
Para diagnosticar la esquizofrenia, un médico utilizará los criterios del Manual diagnóstico y estadístico de los trastornos mentales, quinta edición (DSM-5).
Según los criterios, una persona debe tener al menos dos de los siguientes síntomas durante un mes:
- alucinaciones
- alucinaciones
- habla desorganizada
- comportamiento extremadamente desorganizado o catatónico
- síntomas negativos, como falta de habla, estancamiento emocional o falta de motivación
También deben experimentar un deterioro considerable en su capacidad para funcionar en la escuela o en el trabajo, para interactuar con los demás o para realizar tareas de autocuidado, y deben tener síntomas que persistan durante 6 meses o más.
Puede ser difícil diferenciar entre la esquizofrenia y una afección similar llamada trastorno esquizoafectivo. Este último provoca síntomas similares a la esquizofrenia, pero se caracteriza por un desapego de la realidad más que por una realidad alterada.
Tratamiento (Parte 6 de ¿La esquizofrenia es genética?)
La esquizofrenia es una enfermedad de por vida, pero varios medicamentos pueden ayudar a controlar los síntomas, mejorar la calidad de vida y ayudar a los pacientes a evitar la hospitalización. De acuerdo a Noticias médicas hoy , las opciones de tratamiento incluyen:
- Fármacos antipsicóticos
- risperidona (Risperdal)
- olanzapina (Zyprexa)
- quetiapina (Seroquel)
- ziprasidona (Geodon)
- clozapina (Clozaril)
- haloperidol (Haldol)
- Asesoramiento
- Atención especial coordinada
El Instituto Nacional de Salud Mental puede ser referido para obtener más información sobre el tratamiento, el diagnóstico y las causas de la esquizofrenia.
Si te gustó este artículo, deberías consultar nuestras otras publicaciones en el Biblioteca de investigación de nebulosa !
Puede estar particularmente interesado en nuestros otros esquizofrenia artículos y aquellos sobre otras enfermedades mentales como Enfermedad de Alzheimer y demencia , trastornos que afectar el cerebro como nosotros envejecemos.