Table of contents
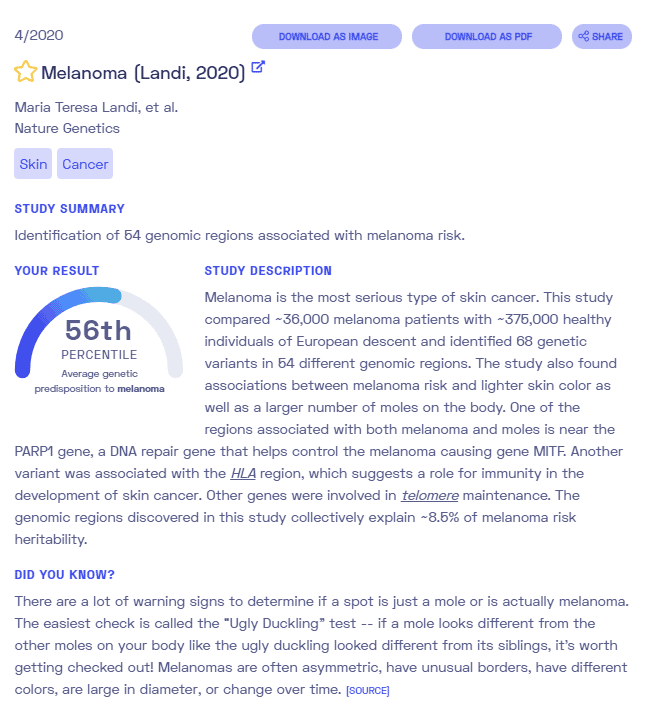
Nebula Genomics DNA Report for Melanoma
Is melanoma genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is Melanoma?
Melanoma, also known as cutaneous melanoma, is a skin cancer that forms in the pigment cells called melanocytes and can appear anywhere on the skin. These cells produce melanin, which gives the skin its color. Many melanomas develop from existing moles. Changes in a mole’s size, edges, color, itchiness, or skin breakdown can indicate a cancer case.
Although not as common, the condition can also form in the eyes or internally in the nose or throat.

Typically, exposure to ultraviolet (UV) radiation, either from the sun or from artificial lamps, as in tanning beds cause the condition. Doctors can diagnose it through biopsy and analysis of skin pigmented lesions that they suspect to be cancerous.
Doctors can successfully treat most cases if they detect it early. Surgery to remove the affected skin area is performed to treat melanoma. In most cases in which the cancer has not spread, surgery results in a cure.
Even though localized cancer has a high survival rate, melanoma is still the most dangerous type of skin cancer. The best way to protect yourself from this condition is by using sunscreen and avoiding direct UV light.
The other two types of skin cancer are squamous cell carcinoma and basal cell carcinoma. Like melanoma, they also occur in the top layer of the skin.
Is Melanoma Genetic?
As a cancer, genetic mutations that either keep on oncogenes (genes that cause cancer) or turn off tumor suppressor genes (genes that prevent cancer) ultimately cause all melanomas. Individuals can either acquire these genetic changes during life or inherited from their parents. The most common genetic variations associated with melanoma are acquired, but a few can be inherited and run in families.
A genetic counselor can help assess your risk, especially if you have a family history of melanoma.
Overall, an inherited mutation that occurs as an autosomal dominant gene causes about 10% of melanomas. This means that the mutation occurs in only one copy of the gene.
About 8% of people diagnosed with melanoma have a first-degree family member with the condition. A much smaller percentage, about 1% to 2%, has two or more close relatives with the disease.
Genes involved
BRAF: This acquired genetic mutation is found in half of all cases. BRAF is an oncogene involved in an important signaling pathway that instructs a cell to grow, divide, move, and destruct.
Cyclin dependent kinase inhibitor 2A (CDKN2A): This gene is needed to produce several proteins, especially the p16 and p14 proteins. These are tumor suppressor proteins.
Changes in tumor supressor genes most often cause familial melanomas. To date, scientists have identified two gene mutations as increasing the risk of familial malignant melanoma: the CDKN2A and CDK4 genes. Both of these genes play essential roles in controlling when cells divide. They may also be associated with pancreatic cancer.
Some people inherit a condition called xeroderma pigmentosum (XP). It involves a change in the XP (ERCC) genes, which generally help to repair damaged DNA inside the cell. DNA in skin cells of these patients has a more difficult time repairing damage after UV exposure, increasing the risk of developing melanoma.
Other genes can also increase your risk of melanoma. For example, people with red hair carry a genetic variant on the gene MC1R that puts them at a high risk of skin cancers equal to 21 years of sun exposure. Those with blue or green eyes are also at higher risk.
Genetic testing and genetic counseling can help you assess whether you may have higher risk factors for developing melanoma.
Current Research on Melanoma
There is plenty of knowledge about this type of cancer, and several studies are underway. Physicians are clear on the effect of BRAF inhibitors (BRAFi) and MEK inhibitors (MEKi). In 2018, the journal Pharmacological Research published cancer research on the Immunomodulatory effects of BRAF and MEK inhibitors and the implications for Melanoma therapy.
This article from 2018 describes the genetics of metastasis of cancers but with a particular focus on melanoma.
A rather unknown and particular type, uveal melanoma, was the object of study in 2019. You can learn more about the genetic evolution of metastatic uveal melanoma in this article from Nature Genetics. You may also want to look at this characterization of genetics in patients with mucosal melanoma, and the treatment applied.
That same year, Genetics in Medicine published an interesting article about the relationship between the genetic markers of pancreatic cancer and melanoma. This study sought to change risk perceptions and, possibly, develop better treatment options.
Epidemiology
According to the Centers for Disease Control and Prevention (CDC), about 83,000 new cases of melanoma occurred in the United States in 2018. It is currently the sixth most common cancer in terms of new cases.
Data between 2012-2016 showed that the highest incidence rate was among non-Hispanic white males, and the lowest rate was among black females. During the same period, about 9,008 people died from the condition in the United States each year.
Although the incidence of cancer has been increasing in the United States, the death rate has declined. Experts attribute this observation to new and more effective treatment options.
Symptoms
Anything unusual on the skin, including moles, lumps, sores, blemishes, markings, or changes in the way an area of the skin looks or feels, can indicate melanoma or other skin cancer.
Experts often associate melanoma with changes in moles on the skin. Most people have some moles either at birth or gained in childhood, and most of them are harmless. Moles tend to be evenly colored, round or oval, and flat or raised.
Warnings
According to the American Cancer Society, the most important warning sign of melanoma is a new spot on the skin or a spot changing in size, shape, or color. You may also notice a spot that is different from the other spots on your skin, known as the Ugly Duckling Sign. You can find more health information on their website.
They also recommend the ABCDE rule for assessing whether a mole could be the sign of melanoma including:
- Asymmetry: One half of a mole or birthmark does not match the other
- Border: The edges are irregular, ragged, notched, or blurred
- Color: The color is not the same all over and may include different shades of brown or black, or sometimes with patches of pink, red, white, or blue
- Diameter: The spot is larger than 6 millimeters across
- Evolving: The mole is changing in size, shape, or color

If you notice any of these changes, it is important to talk with your doctor. You should also be aware of the slight chance of melanomas occurring on areas other than the skin, including under nails, inside the mouth, or in the eye. Acral lentiginous melanoma is a rare type that appears on the soles of the feet or palms of the hand.
It can be difficult to distinguish normal moles from cancerous ones, especially in areas that are difficult to see, which is why it’s important to speak with a healthcare professional at the first warning sign. Most cases that are diagnosed early can be treated.
Cause
Experts are unsure why some moles and spots become cancerous while most others do not. Several factors may put certain groups of people at greater risk. In most cases, these risk factors cause acquired genetic mutations, changes in the DNA that occur over a lifetime and are not passed down to children.

Environmental risk factors also play a role. The most significant risk factor for melanoma is direct exposure to UV light that damages DNA in skin cells. This damage can cause some genes to no longer function correctly, leading to cancer. Sources of UV light are the sun and artificial light, like tanning beds.
Many people who develop melanoma and other skin cancers do so years after exposure. For example, many children and young adults are exposed to a lot of sunlight which only appears as melanoma later in adulthood. Sunscreen is a proven protection against the damaging side effects of UV light and everyone should use it as recommended, even on cloudy days.
Having fair skin, a history of skin cancer, or a weakened immune system also increase melanoma susceptibility.
Diagnosis
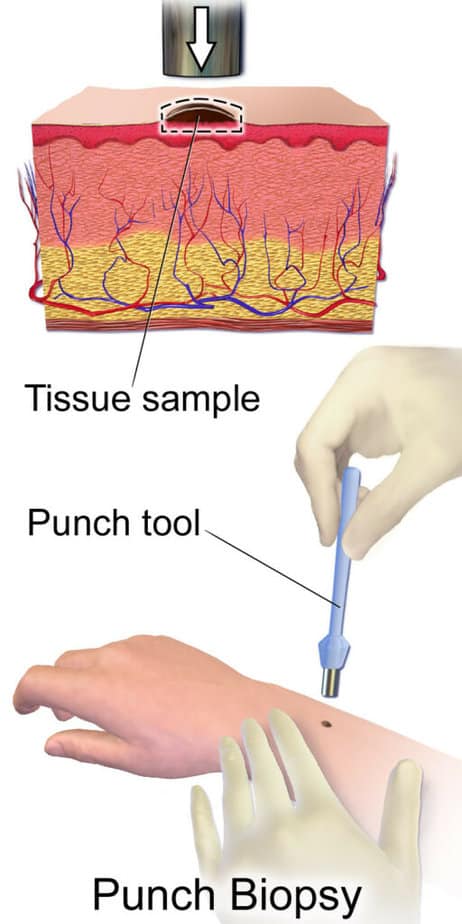
Doctors initially diagnose melanoma through a skin examination. Abnormal spots or moles are the first signs of the condition. If an area seems suspicious, your doctor will normally perform a skin biopsy to confirm the presence of skin cancer. This procedure involves taking a skin sample and analyzing it in a lab.
Usually, a doctor removes the whole growth either through a punch biopsy (a circular blade pressed against the skin) or excisional biopsy (a scalpel that removes the entire mole).
If a biopsy determines the presence of melanoma, your doctor will recommend additional tests to determine the cancer’s extent.
Thickness tends to be an indicator of how serious the cancer is. While a doctor can remove thinner cases with surgery, a thicker case may indicate more severe disease or cancer spread.
If the doctor suspects the cancer has spread to the nearby lymph nodes they may perform a sentinel lymph node biopsy. During this procedure, a doctor injects a dye at the site where the cancer was present. It will eventually leak into distant lymph nodes, of which a sample is removed. If the dyed lymph node does not contain cancer, it is unlikely to spread to other nodes.
In more severe cases, imaging tests like X-rays, CT scans and positron emission tomography (PET) scans can search for cancer in other parts of the body. The medical professional will not usually perform these tests when the melanoma is small and unlikely to spread past the skin.
Stages
Doctors diagnose stages of melanoma as I through IV. The early stages 0-I are easily treatable, while stage IV indicates that the cancer has metastasized to other parts of the body. The stage of the cancer largely determines diagnosis and treatment.
Doctors may also use a lactate dehydrogenase (LDH) test, which is an indicator of disease prognosis.
Treatment
Treatment of melanoma will depend on a number of factors such as the type, stage of the cancer, the patient’s overall health, and personal preference.
The only treatment needed for small and very thin melanomas may be to remove the affected area through biopsy. Removing the cancer will generally cure the condition.
A patient may need more advanced treatment if the cancer has spread beyond the skin. These options may include:
Surgery
Doctors may recommend surgery to remove the affected lymph nodes as well as additional treatment.
Immunotherapy
Doctors may recommend this treatment after surgery if the cancer has spread, especially if they cannot remove the melanoma completely. There are different options for immunotherapy although they all help the body’s immune system better recognize cancer cells and destroy them.
Targeted therapy
This is another treatment that may be recommended after surgery if the cancer has spread. This medicine takes advantage of targeted specific weaknesses on cancer cells and destroys them in areas far away from the skin.
Radiation therapy
This therapy is normally used for cancer that is not able to be removed completely with surgery. It involves using high-powered energy beams, such as X-rays and protons, to kill cancer cells. It can also help relieve symptoms as well as treat the disease.
Chemotherapy
This treatment uses medications designed to kill cancer cells. These drugs can be given either intravenously or orally.
If you liked this article, you should check out our other posts in the Nebula Research Library!
June 15, 2023
