Table of contents
Nebula Genomics DNA Report for Eczema
Is eczema genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!
What is Eczema?
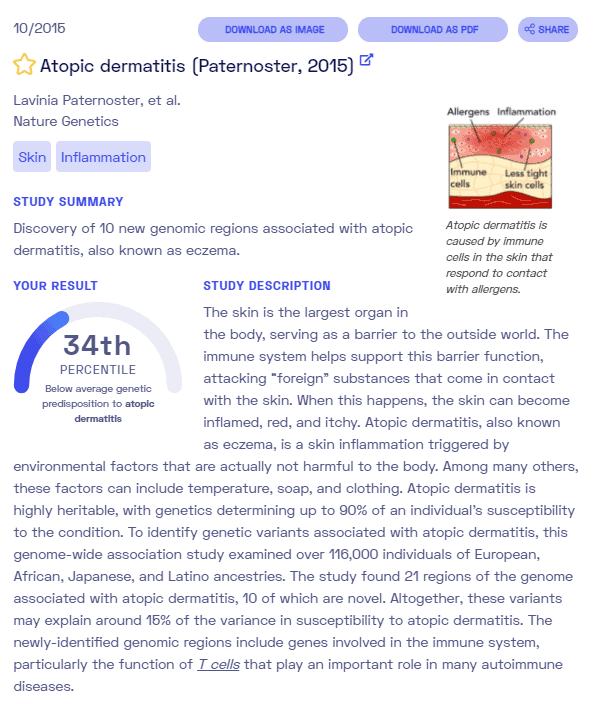
Dermatitis is the general term for any type of skin irritation. Eczema, or atopic dermatitis, is a long-term type of inflamed skin characterized by dry, itchy skin that may also appear red and swollen or weep clear fluid. Atopic eczema is not contagious.
Atopic dermatitis is the most common type of eczema. Other forms include contact dermatitis, dyshidrotic eczema, nummular eczema, seborrheic dermatitis, and stasis dermatitis.
Eczema is an autoimmune disease turned on when an allergen from outside of the body turns on the immune system, attacking healthy cells. As a result, the affected cells become inflamed, which leads to the dry, itchy skin that characterizes the condition.

Although it can appear at any time, the condition normally begins in childhood and changes in appearance depending on age. It is most common on most of the body during infancy (less than one year of age).
This includes the face, scalp, hands, and feet. In adolescents, the knees and elbows are most affected. In adults, the rash tends to affect the neck and eyelids as well as knees and elbows.
It can be very common in infants, but children may see significant improvement with age.
Although there is no cure for the condition, there are multiple treatment options. Most treatments involve a topical application to ease symptoms and reduce inflammation of the skin.
Is Eczema a Genetic Disease?
In most cases, the interaction of several genes causes the condition, in addition to an environmental trigger. In rare cases, a single genetic variation for eczema appears to be the leading cause.
CARD11: This gene codes for a protein that turns on signaling pathways involved in the development and function of lymphocytes in the immune system. When this gene is mutated, T cells, which protect the body from infection, do not function properly. Specifically, they do not respond as strongly to foreign invaders and thus weaken the immune system and result in frequent infections.
Although experts believe several genes are involved, each only contributes a small genetic risk of developing atopic eczema. They have linked the strongest association to a genetic mutation that affects the skin’s ability to form a healthy protective barrier against allergic reactions and irritants.
FLG: This gene is mutated in 20 to 30 percent of people with the condition compared with 8 to 10 percent of the general population. It codes for a protein called profilaggrin, an essential component of the outer skin. The skin is a barrier that keeps water in and foreign substances like toxins, bacteria, and allergens out.
When this gene is abnormal, the profilaggrin tends to be too short, an effect that reduces the protein’s ability to create additional structures in the skin. Without a strong barrier, experts believe that allergens enter the skin and trigger the inflammatory response observed in the condition.
Since not everyone with an FLG mutation develops genetic eczema, environmental conditions most likely play a role as well.
Other genetic factors probably play a role in the skin barrier or the immune system.
Current Research on Eczema
Eczema has become the topic of study of many institutions, and a lot has been discovered so far. This 2018 study sheds light on genetic studies that have tried to identify the genes responsible for several conditions, eczema included. Two years before that, scientists had tapped into the genetics and epigenetics of atopic dermatitis.
This exhaustive study goes deeper into germline hypomorphic CARD11 mutations in severe atopic disease. Eight patients with novel heterozygous mutations in CARD11 underwent a series of tests to determine the relationship between eczema and the type of genetic mutation associated with it.
Topical treatments like emollients and moisturizers have proven certain effectiveness at controlling eczema and preventing eczema flares. This 2020 study has mixed results based on subject experience about how well moisturizers help diminish pesky eczema symptoms.
On the other hand, a Cochrane Library assessment of the effects of probiotics for the treatment of eczema proved that their use makes little difference in patients. Therefore, they conclude that the use of probiotics is not based on evidence.
Patients in general claim to suffer from mild eczema on hands, and others might perceive it as severe. There really isn’t a metric to classify the severity of hand eczema. However, these authors devised a classification based on the guideline of the Danish Contact Dermatitis Group.
Epidemiology
According to the Allergy and Asthma Network, eczema affects 31.6 million people in the United States. Out of that number, 18 million people have atopic dermatitis (AD), including 9.6 million children.
Globally, 15-20% of children and 1-3% of adults are thought to have AD.
The condition appears to affect male and female children to the same extent, but more female adults have it overall than males. It tends to affect people of all races and nationalities, although the risk appears to be smaller in children of Hispanic descent than those of other races.
Symptoms
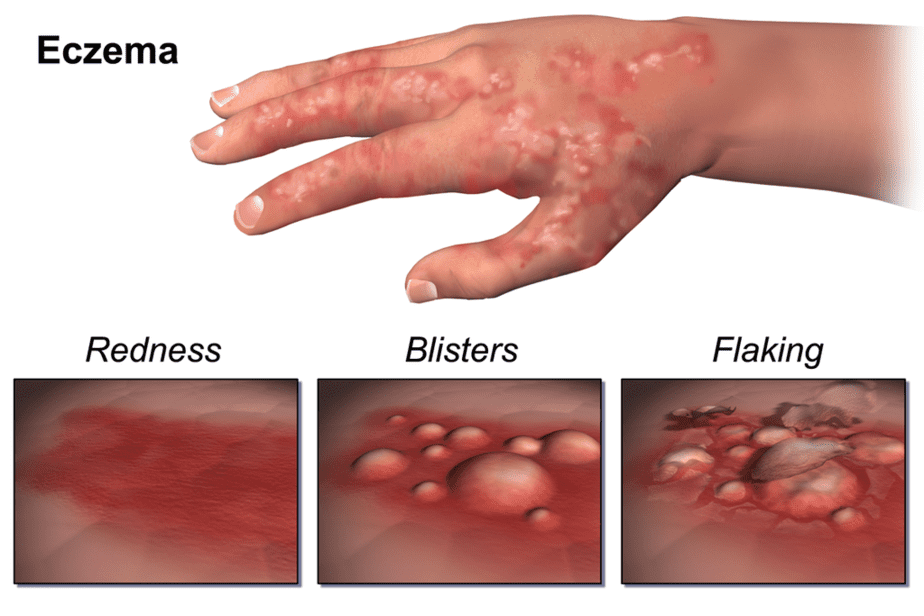
The symptoms of eczema are different for each patient. You may even observe different signs on different parts of your body.
The American Academy of Dermatology Association summarizes the symptoms by age on their website. A common symptom is itchy skin, which can range from mild to severe and often worsens at night, reducing sleep and negatively impacting quality of life. Scratching tends to make the skin conditions worse. Other symptoms to look for include:
- Dry, sensitive skin
- Inflamed, discolored skin
- Rough, leathery, or scaly patches of skin
- Oozing or crusting
- Areas of swelling
The condition often occurs as flare-ups, in which the symptoms are present for a while and then go into remission, a time in which no symptoms are present. Some patients experience remission for up to several years.
People with atopic eczema tend to have other allergic conditions such as asthma and hay fever. They may also be at higher risk for skin infections (when repeated scratching breaks the skin), irritant hand dermatitis, and allergic contact dermatitis.
There may also be an increased risk of other inflammatory disorders, including inflammatory bowel disease (Crohn’s disease and ulcerative colitis), rheumatoid arthritis, and hair loss caused by a malfunctioning immune reaction (alopecia areata). In addition, children may experience behavioral complications such as ADHD and depression.
Causes
Although the cause of eczema is unknown, experts largely believe it is a combination of genetic and environmental factors (such as living with a pet). The condition results when immune cells are turned on in response to an outside allergen and causes inflammation in the skin.
Some of the most common eczema triggers listed by the National Eczema Association include:
- Dry skin
- Irritants such as
- metals (especially nickel)
- cigarette smoke
- soaps and household cleansers
- fragrances
- certain fabrics like wool and polyester
- antibacterial ointments like neomycin and bacitracin
- formaldehyde (found in household disinfectants
- some vaccines
- glues and adhesives
- isothiazolinone, an antibacterial found in personal care products like shampoos
- Cocamidopropyl betaine (used to thicken shampoos and lotions)
- paraphenylenediamine (used in leather dyes and temporary tattoos, among others)
- Stress

Dyron via Wikipedia. CC-Attribution-Share Alike 3.0 Unported
The greatest risk factor in developing eczema is having a family history of the disorder or a history of allergies (including food allergies), hay fever, or asthma.
Diagnosis
A specialist who observes your skin and symptoms often diagnoses the condition. The doctor will look for the classic signs of redness and dryness. Usually, this is enough for a diagnosis. However, your doctor may order other tests if they need to rule out other conditions or have other concerns.
- An allergy skin test
- Blood tests to check for causes of the rash that might be unrelated to dermatitis
- A skin biopsy to distinguish one type of dermatitis from another
Treatment
Does eczema go away eventually? As mentioned earlier, this chronic skin disease has no cure, but patients can keep it under control. Options for treating eczema are available, although their effectiveness varies between patients. How long does eczema last will depend on consistent treatment and the patient’s particular response.
Some changes to your daily routine and skin care may significantly improve your symptoms. Many of them focus on moisturizing your skin.
- Using a humidifier in dry environments
- Creams and ointments that seal in moisture such as petroleum jelly
- Using mild soaps, detergents, and other products that are free of perfumes, dyes, and alcohol. These products are usually labeled as “fragrance-free,” “hypoallergenic,” or “for sensitive skin.”
- Using skin products that contain ceramide
- Taking over the counter cortisone creams and ointments and/or antihistamines
- Taking special baths such as oatmeal, salt water, vinegar, and bleach baths
- After bathing, gently pat the skin dry instead of rubbing
If moisturizing and over the counter skin care products are not enough, a health care professional may recommend the following options summarized on Mayo Clinic:
Medications
Prescription creams: These are usually a prescription corticosteroid cream or ointment. It’s important to follow the instructions as overuse may cause side effects, including stretch marks that may become permanent.
Other creams may contain drugs called calcineurin inhibitors that affect your immune system. People older than age 2 can use these products to help control the skin reaction. You should avoid strong sunlight when using these products.
Antibiotics: Your doctor may prescribe an antibiotic cream if your skin has a bacterial infection or if there are open sores or cracks from scratching.
Oral corticosteroids: These drugs are effective but can’t be used long term because of potentially serious side effects. They usually are only prescribed in the most severe cases.
Biologics: The Food and Drug Administration (FDA) has recently approved a new, injectable drug for the condition called dupilumab (Dupixent). It is used for severe cases that do not respond well to other treatment options. Studies have shown it to be safe if used as directed. It is very expensive.
Light therapy
If medications are not effective, your doctor may recommend a type of light therapy that exposes the skin to different kinds of light. One option is phototherapy, in which the skin is exposed to controlled amounts of natural sunlight. Other forms include artificial ultraviolet A (UVA) and narrow-band ultraviolet B (UVB). These treatments can be used alone or in combination with medication.
Side effects of this treatment include accelerated skin aging and an increased risk of skin cancer, so it is important to speak with your doctor regarding this therapy. Because of these risks, it is rarely recommended for children and never provided for infants.
Infants and young children
For infants, the treatment options are more limited and may include:
- Identifying and avoiding skin irritants, including in clothing and laundry detergent
- Avoiding extreme temperatures
- Skin lubrication with bath oils, ointments, or creams
If the condition does not improve, some pediatricians may prescribe prescription-strength medication to help.
If you liked this article, you should check out our other posts in the Nebula Research Library, including those that cover psoriasis and acne. You may also be interested in the National Institutes of Health’s website.
March 31, 2023
