Table of contents
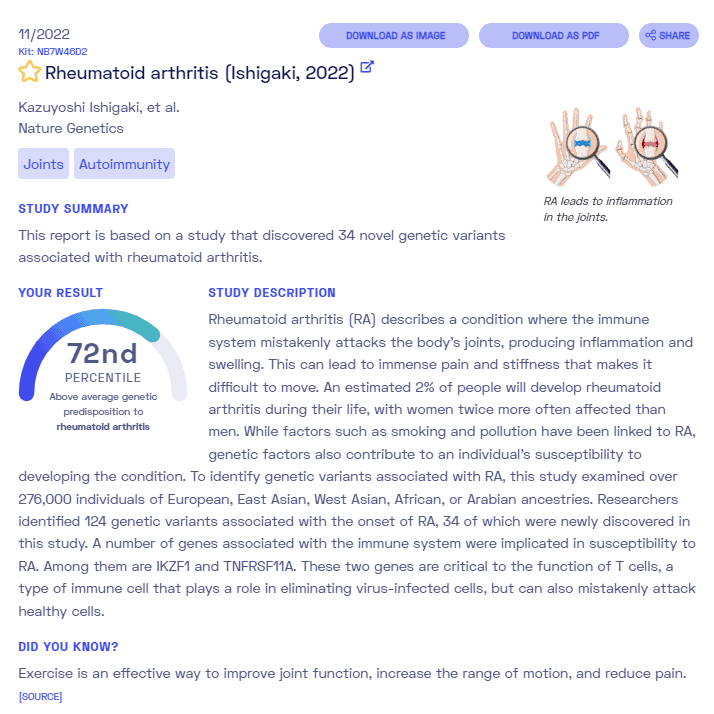
Nebula Genomics DNA Report for Rheumatoid Arthritis
Is rheumatoid arthritis genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!
What is Rheumatoid Arthritis?
Rheumatoid arthritis is a long-term, persistent rheumatic disease and the most common inflammatory disease of the joints. Inflammatory arthritis is often abbreviated as RA.
RA is an autoimmune disease, meaning that the body’s immune system attacks healthy cells by mistake, leading to symptomatic inflammation. In this case, antibodies attack the healthy lining of joints.
The onset of the disease is often gradual but can also be sudden, with pain in the joints of the little fingers or toes. It may also affect other joints, especially hand, knee, shoulder, foot, hip joints.
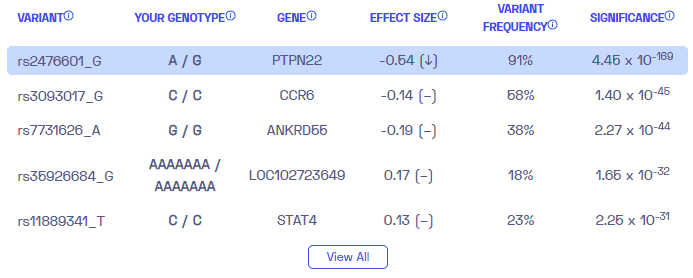
Typically, it specifically affects the carpal bones, the metacarpophalangeal joints of the fingers, and the proximal interphalangeal joints (PIP). The finger end and toe end joints (distal interphalangeal joints, DIP) are not affected, unlike psoriatic arthritis. The condition causes pain when the it leads to inflammation of the joint lining and damage to the joint tissue.
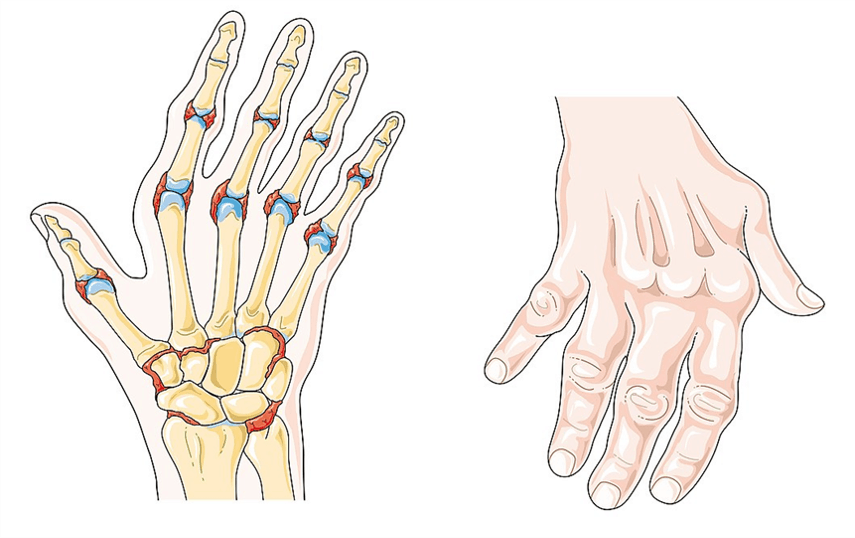
Swollen joints overheat and may appear red as a result. Patients also often experience joint deformity. Symmetrical synovitis of the truncal joints is typical.
These symptoms are usually most pronounced in the morning, causing what most patients describe as morning stiffness. As the disease progresses, it affects more and more joints.
The disease usually progresses in episodes that typically last between a few weeks and months. Between the individual relapses, the symptoms subside on their own.
Did you know you can test inflammation markers at home? Learn more in our article about at home inflammation tests.
Is Rheumatoid Arthritis Genetic?
Those who have a parent, sibling, or offspring with the condition have a prevalence rate of 2 to 3%. On the other hand, the rates of the condition if one identical twin has the condition are as high as 15 to 20%. There are several genetic markers and over 100 regions in the genome known to be associated with the development of rheumatoid arthritis. Research continues to identify genetic components.
Human leukocyte antigen (HLA) genes (i.e., HLA-DR4): Also called the major histocompatibility complex, MHC, this gene is most strongly associated with an increased risk of developing rheumatoid arthritis. Patients with this genetic variant also tend to have more severe symptoms.
STAT: This gene regulates and activates the immune system.
TRAF1 and C5: These genes play a major role in causing chronic inflammation.
PTPN22: This gene helps regulate signal transduction that controls the activity of immune system cells called T cells. It influences the progression and expression of a number of diseases, including rheumatoid arthritis.
Current Research on Rheumatoid Arthritis
There has been much research on rheumatoid arthritis RA and its relationship with genetics of rheumatoid arthritis. Studies have shown that excluding environmental factors, people with a family member suffering the disease are more likely at risk of rheumatoid arthritis.
Genetics
A 2016 study carried out by the British Society for rheumatology gave a full description of the role of genetic aspects developing rheumatoid arthritis.
The study captured all of the genes responsible for RA and confirmed that based on identical twins studies, 60% of the cause of rheumatoid arthritis is generally based on genetics.
The study revealed the Human Leucocyte antigen HLA-DRB1 as the largest genetic risk factor for RA. Authors also identified other genes correlated with rheumatoid arthritis risk, such as HLA-DR, STAT, and PTPN22.
A 2018 study published in the Journal of Laboratory Precision Medicine revealed that genetic factors plays an important role in the pathogenesis of rheumatoid arthritis.
Through large clinical cohorts, the authors demonstrated that there are more than 100 genes associated with rheumatoid arthritis. The Human Leukocyte Antigen- HLA-DRB1 gene, one of the first genes to be identified, is strongly related to increased risk within families. In particular, the HLA-DRB1 01, HLA-DRB1 04, and HLA-DRB1 10 alleles are highly correlated with a high risk of developing rheumatoid diseases in ACPA positive patients where ACPA stands for Anti citrullinated peptide/protein bodies.
The reason for this correlation is because these three HLA-DRB1 alleles share an identical amino acid sequence, also known as Shared Epitope (SE), in the peptide-binding groove.
The study cited other HLA-DRB1 alleles like the HLA-DRB1 03, HLA-DRB1 07, HLA-DRB1 11, and HLA-DRB1 13 that play a role in the disease as protectors. The HLA-DRB4 gene was also revealed to increase the risk of the disease activity.
Finally, the study cited other non-HLA genes to be strongly associated with the risk of developing the disease, including various SNPs, STAT-4, and interleukin (IL-10).
Twin studies
A more recent study carried out in 2021 by the National Rheumatoid Arthritis Society reported that first-degree relatives of people with rheumatoid arthritis (parents or siblings) were three times more likely to develop rheumatoid arthritis than first-degree relatives of people who do not have the condition.
To determine how much genetics increases the risk of developing RA, the study compared identical twins who share 100% gene makeup to non-identical twins with 50% gene makeup. The results showed that identical twins were 15% more likely to have the condition, while non-identical twins were 4% likely to have RA. They estimated that genetic factors accounted for 53 to 68% of the causes of the condition.
Epidemiology
Rheumatoid arthritis (RA) affects nearly 1% of adults worldwide. As of 2019, the incidence of new cases ranged from 5 to 50 per 100 000 adults in developed countries, with risk increasing with age. That’s equivalent to about 1.5 million people living with rheumatoid arthritis in the United States.
Rheumatoid arthritis affects women three times as much as men. Although individuals of any age can develop it, the average age of the condition is around 66 in the United States. Geographically, it is most prevalent in North America and Northern Europe.
Causes
Rheumatoid arthritis occurs when the body’s immune system attacks the lining of joints, leading to inflammation. Genetic and environmental factors often both contribute to its progression. It is not certain what triggers this autoimmune reaction, but a genetic component most likely plays a role. A number of environmental risk factors associated with the disease. For those predisposed to rheumatoid arthritis via genetics, the disease may be more easily triggered if exposed to external contributing factors such as bacteria, viruses, emotional stress, etc.
Mayo Clinic lists some additional risk factors that may make individuals more susceptible to the disease:
- Your sex. Women are more likely than men to develop the condition
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins in middle age
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease
- Smoking. Cigarette smoking increases your risk, especially if you have a genetic predisposition towards the condition. Smoking may also be associated with greater disease severity
- Environmental exposures. Some exposures, such as asbestos or silica, may increase the risk.
- Obesity. Overweight or obese People — especially women age 55 and younger — may be at a slightly higher risk
Symptoms
In the early stages, people with rheumatoid arthritis may not see redness or swelling in the joints, but they may experience tenderness and pain. The effects of the condition normally begin in the smaller joints (those that attach the fingers to the hand, for example) before expanding to the larger joints (knees, ankles, and shoulders). Rheumatoid arthritis usually occurs on both sides of the body.
Late stage symptoms of rheumatoid arthritis include:
- Joint pain and swelling, tenderness, or stiffness lasting for six weeks or longer.
- Morning stiffness lasting for 30 minutes or longer.
- More than one joint is affected.
- Small joints (wrists, certain joints in the hands and feet) are typically affected first.
- Pain on the same joints on both sides of the body.
- Many people with RA get easily exhausted (fatigue), and some may develop a low-grade fever. RA symptoms may come and go. Having a lot of inflammation and other symptoms is called a flare and can last for days or months.
Rheumatoid arthritis is a chronic condition. Signs and symptoms appear periodically as a series of flares and remissions. The symptoms can lead to loss of function if severe enough. It may also affect non-joint parts of the body such as skin, eyes, lungs, heart, blood vessels, and bone.
You should check with your doctor if you notice new signs and symptoms.
It also increases your risk of developing other conditions such as osteoporosis, rheumatoid nodules (firm bumps of tissue), dry eyes and mouth (including Sjögren’s syndrome), infections, abnormal body composition, carpal tunnel syndrome, heart problems, lung disease, and lymphoma (a type of blood cancer).
Diagnosis
Rheumatoid arthritis can be difficult to diagnose in the early stages before the symptoms are more pronounced. There is no substitute for professional medical advice. During a physical examination, if you suspect you have rheumatoid arthritis, your doctor will most likely check your joints for swelling, redness, and warmth. They may also check reflexes and muscle strength.
If your doctor suspects the presence of the condition, they will most likely refer you to a specialist called a rheumatologist.
Blood tests
A person with rheumatoid arthritis will often have elevated substances in their blood compared to someone without the condition. For example, elevated erythrocyte sedimentation rate (ESR, or sed rate) signals too much inflammation in the joints. Elevated C-reactive protein (CRP) may indicate a non-specific inflammatory process. Other common blood tests look for rheumatoid factor (a blood protein) and anti-cyclic citrullinated peptide (anti-CCP) antibodies (pieces of protein).
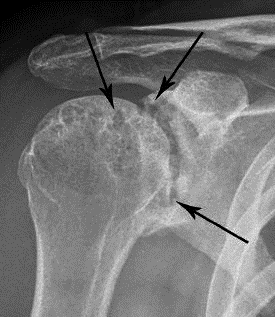
Imaging tests
Doctors use these tests, such as X-rays and MRIs, to track the progression of the disease over time. Doctors will order these tests periodically to determine how much damage has occurred in the affected joints.
Treatment
While there is no cure for rheumatoid arthritis, the symptoms can usually be managed through medication and therapy. If these approaches do not work, it may be possible to repair the joints through surgery.
Medications
NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) relieve pain and reduce inflammation. Some common non-prescription NSAIDs for RA include ibuprofen (Advil, Motrin IB) and naproxen sodium (Aleve). Your doctor may prescribe a stronger prescription NSAID. Side effects may consist of stomach irritation, heart problems, and kidney damage.
Steroids: Corticosteroid medications reduce inflammation and pain and slow joint damage. Side effects may include thinning of bones, weight gain, and diabetes. Steroids are generally not intended to act as a long-term solution. Instead, they are often prescribed to relieve immediate symptoms and then substituted with a different treatment.
Disease-modifying antirheumatic drugs (DMARDs): These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Side effects vary but may include bone marrow suppression, liver damage, and severe lung infections.
Biologic agents: Also known as biologic response modifiers, these drugs can target parts of the immune system that trigger inflammation causing joint and tissue damage. Anti-TNF therapy is an antibody that is used widely. These types of drugs also increase the risk of infections and blood clots in the lungs. In general, biologic DMARDs are most effective when combined with a nonbiologic DMARD, such as sulfasalazine.
Therapy
Physical or occupational therapy can help treat rheumatoid arthritis patients by giving them more flexibility of their affected joints through targeted exercise. Arthritis care and effective treatment may also include changes to daily routines or assistive devices that would reduce the reliance on those joints. For example, some companies make special gripping devices on everyday objects like knives for people with the condition.
Surgery
Surgery may help restore your ability to use your joint. It can also reduce pain and improve function. It is usually only used as a final treatment option when the effect of the condition cannot be successfully treated with medications.
Synovectomy: This surgery removes the inflamed lining of the joint (synovium). It is most common on larger joints such as the knees, elbows, wrists, fingers, and hips.
Tendon repair: Inflammation and joint damage may cause tendons around your joint to loosen or rupture. This surgery is used to repair the tendons around your joint.
Joint fusion: Surgically fusing a joint can stabilize or realign a joint. It can also be used for pain relief when a joint replacement isn’t an option.
Total joint replacement: During joint replacement surgery, the surgeon removes the damaged parts of your joint and inserts a prosthesis made of metal and plastic.
More resources for patients and caregivers can be found on the American College of Rheumatology website.
Osteoarthritis vs. Rheumatoid Arthritis
Although these two conditions both affect the joints, they are very different types of arthritis. Rheumatoid arthritis is an autoimmune disorder that affects the whole body, while osteoarthritis is a degenerative joint disorder that affects only joints if they’ve been damaged.
Patients will often experience similar symptoms, including stiff and painful joints, limited range of motion, tenderness and swelling at the affected joints, and increased feeling of symptoms in the morning.
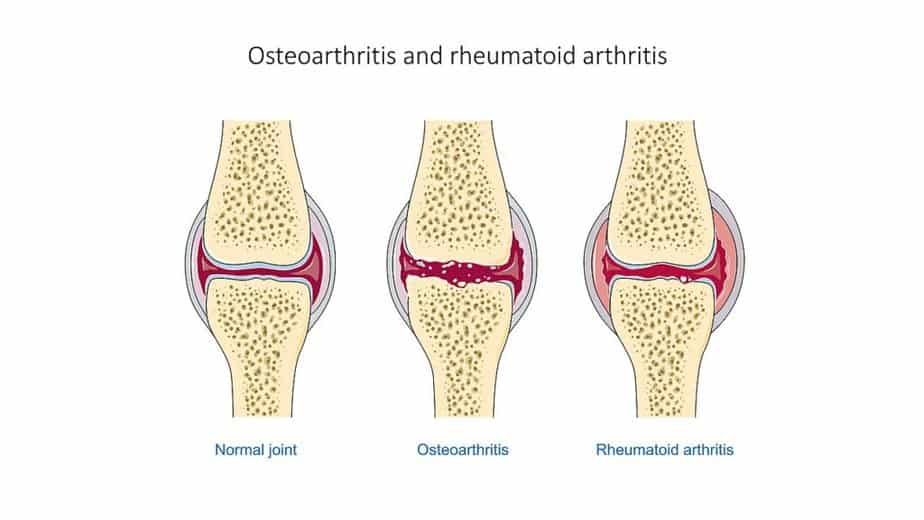
Since rheumatoid arthritis is a broad autoimmune disorder, it also comes with symptoms that affect the whole body, such as fever and muscle aches, as well as detrimental symptoms in the lungs, eyes, and heart. Patients with osteoarthritis lack these broad symptoms since the disorder is limited strictly to the joints. They tend to grow excess bone at the edges of the joints, a condition known as bone spurs.
Osteoarthritis is also less symmetrical than rheumatoid arthritis, sometimes affecting only one side of the body or affecting one side of the body more. Although there is no cure for either, treatments are available to manage the symptoms of both conditions.
If you liked this article, you should check out our other posts in the Nebula Research Library, including those on other autoimmune disorders such as Addison’s disease, MS, psoriasis and lupus.
April 11, 2023
