Table of contents
Nebula Genomics DNA Report for MS
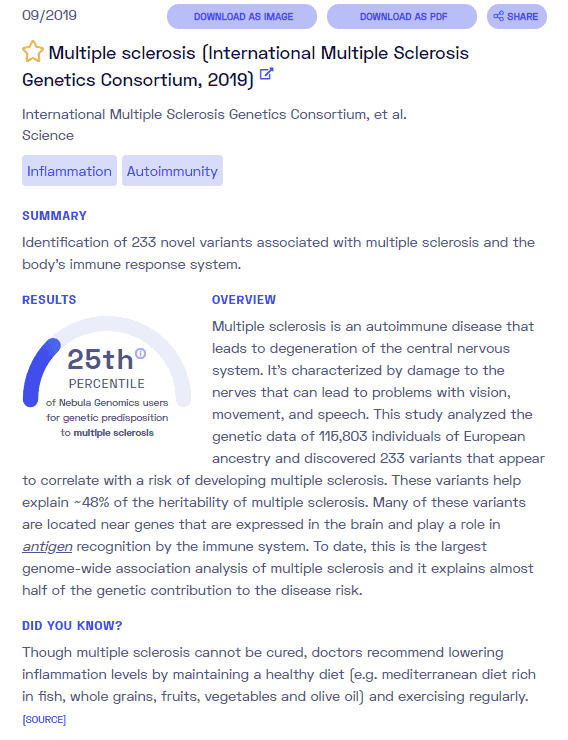
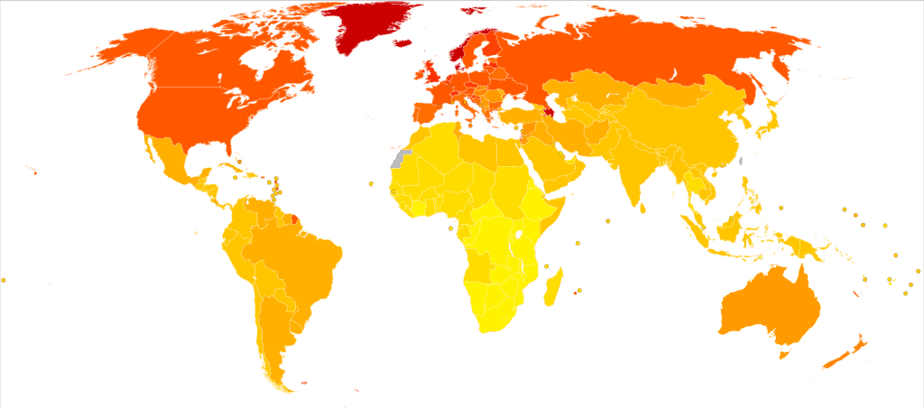
Is MS genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!
| This information has been updated to reflect recent scientific research as of April 2021. |
What is MS?
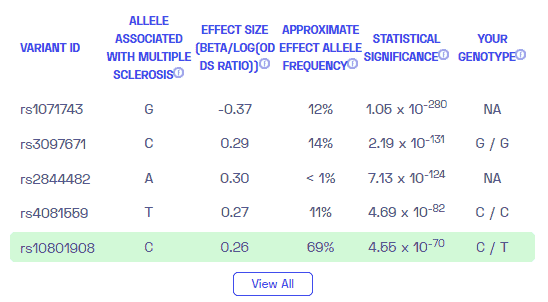
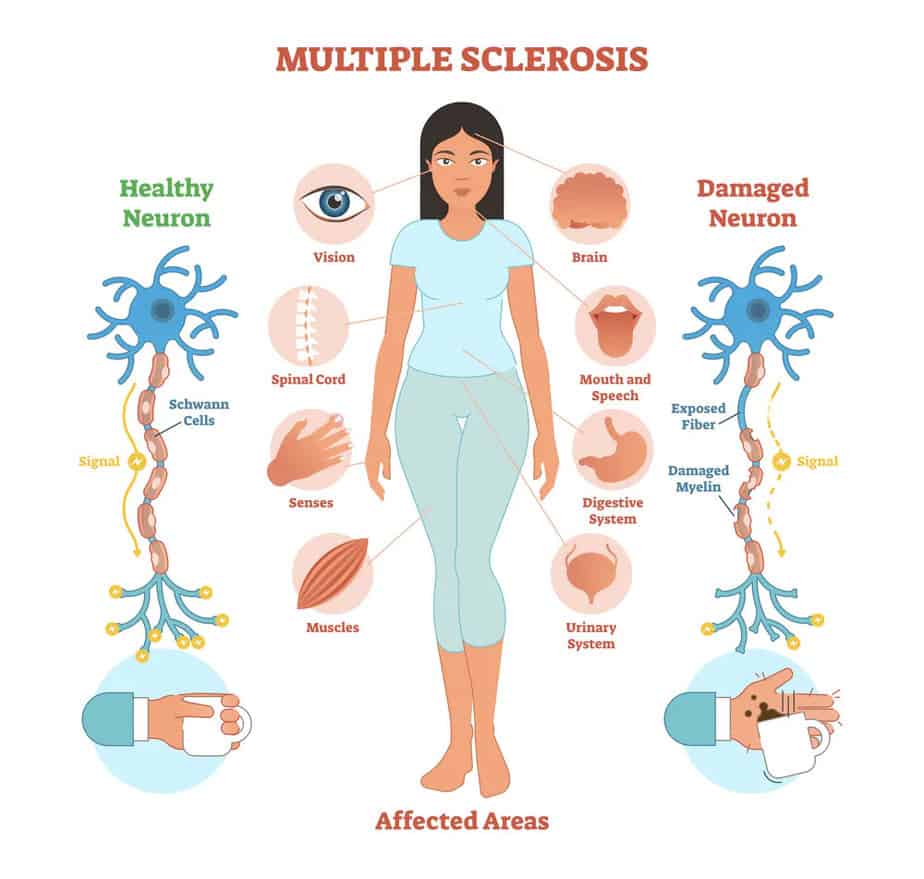
Multiple sclerosis (MS) or encephalomyelitis disseminata (ED) is a chronic inflammatory neurological autoimmune disease with very different forms of progression, depending on the area of nerve damage, the extent, and the severity of the disease.
In general, it affects the central nervous system (CNS). Specifically, it affects the brain and spinal cord by attacking the myelin sheaths that cover them. Myelin sheaths are insulating layers that protect nerves.
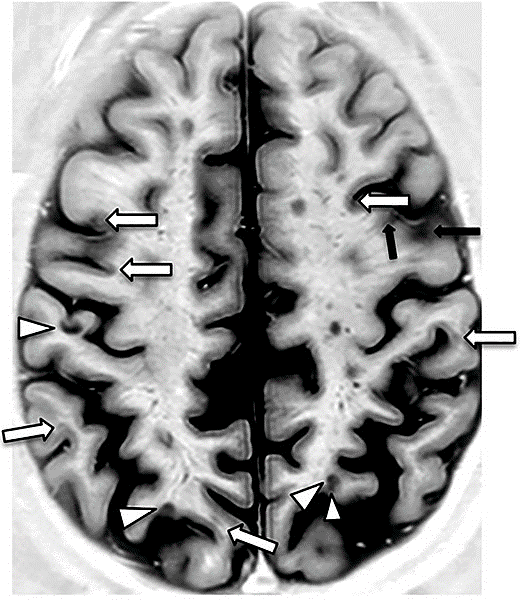
The attacks cause small inflamed patches (plaques or lesions) to appear in the myelin sheath, which doctors can see on an MRI scan. Disruption of messages sent along the nerves causes MS symptoms.
Did you know you can test inflammation markers at home? Learn more in our article about at home inflammation tests.
Types and Causes of MS
There are two main types of MS: primary progressive MS, in which neurological functions gradually worsen with time without relapses or periods of remissions characterize the disease, and relapse-remitting multiple sclerosis, in which symptoms tend to occur in different episodes or relapses. Secondary progressive MS follows an initial relapsing-remitting course.
The exact causes of the disease have not yet been clarified despite research efforts. In MS, experts observe many (multiple) inflammatory demyelination foci scattered in the white matter of the brain and spinal cord, presumably caused by the attack of the body’s own immune cells on the myelin sheaths of the nerve cell processes. Since the centers of demyelination can occur throughout the entire CNS, multiple sclerosis can cause almost any neurological symptom.
Visual disturbances and blurred vision can eventually lead to blindness and eye-movement disorders (internuclear ophthalmoplegia). These are not specific for multiple sclerosis, though.
Along with epilepsy, MS is one of the most common neurological diseases in young adults. There is no cure for the disease, but various measures can favorably influence its course. Multiple sclerosis does not necessarily lead to severe disabilities.
Is MS genetic?
Although the exact cause of MS is unknown, most experts believe that a combination of genetic and environmental factors acts as a trigger for the characteristic immune-mediated damage.
Is MS a genetic disease? As of October 2013, researchers have identified 110 genetic variations that occur more frequently in MS patients than in the general population and may contribute to a predisposition to multiple sclerosis.
More recent estimates suggest that over 200 genes may play roles in development of the condition. Each of these variations alone represents only a shallow risk of developing multiple sclerosis. Together, though, they account for about 20 percent of the genetic components of the disease. Thus, identifying gene variants such as those on HLA-DRB1 and IL7R through genetic tests may help identify individuals most at risk.
Among other things, experts believe that polymorphisms of interleukin signaling pathway genes are involved. Many of the gene variants found are directly related to the immune system. Experts also identify them as genetic risk factors in autoimmune diseases such as diabetes type 1 or Crohn’s disease.
According to the National Multiple Sclerosis Society, the general population’s risk of developing MS is about 1 in 750 – 1000. In identical twins, if one twin has MS, the chance that the other twin is about 1 in 4. The risk of developing MS also increases when other first-degree relatives (parents, siblings, and children) have the condition, but far less than in identical twins.
Research is ongoing to better understand multiple sclerosis genetics and other factors that contribute to the development of MS.
Current Research on Genetic MS
As of 2021, the FDA has approved a series of medications for the treatment of multiple sclerosis. This study from 2019 describes Progressive multiple sclerosis: latest therapeutic developments and future directions. In March of this year, the FDA also approved the use of PONVORY for adult with relapsing multiple sclerosis.
Other alternatives to drugs are in the works for the treatment of this condition. This Cochrane Library article reveals how promising stem cell therapy is looking. Stem cell therapy has shown tremendous progress since research first began more than 15 years ago.
But there are still conditions in affected people that need to be addressed to help improve their lifestyle. Due to neurodegeneration, one major concern is the falls that a patient may suffer, which might lead to injuries and even hospitalization. Take a look at this very recent article on predicting falls and injuries in people with multiple sclerosis using machine learning algorithms.
There has been some discussion regarding patients with MS and vaccines. The National Multiple Sclerosis Society has provided guidance for patients taking the COVID-19 vaccine.
To get the most recent health information, research news, and progress on MS, take a look at the National Multiple Sclerosis Society website.
Non-genetic risk factors
Experts suspect there are multiple non-genetic factors that bring on MS.
Infection
Doctors attribute numerous viruses (including Epstein-Barr virus and human herpesvirus 6) as having a possible role in the development of disease. In fact, an immune reaction against the Epstein-Barr virus is more frequently detectable in children with multiple sclerosis in particular than in children who do not suffer from the disease. Doctors have also associated bacterial pathogens (including chlamydia, spirochaetes, rickettsia, and Streptococcus mutans) with the development of multiple sclerosis.
Vitamin D
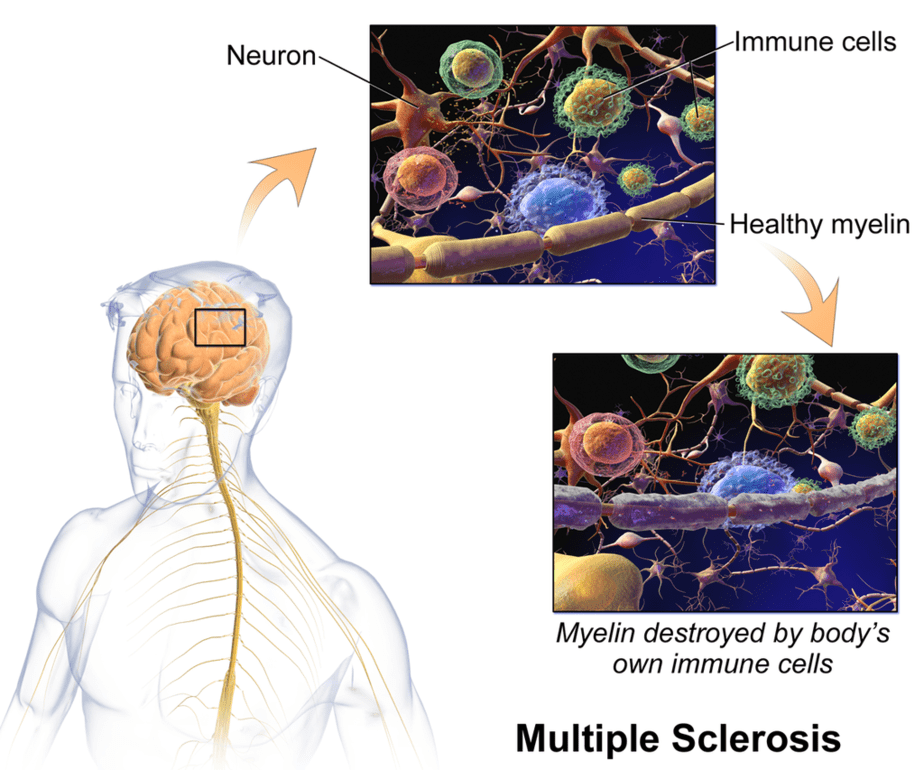
Growing evidence suggests that levels of vitamin D plays a vital role in MS. Specifically, doctors have identified low vitamin D levels in the blood as a risk factor for MS development.
Some researchers believe that sun exposure (the natural source of Vitamin D) may help to explain why people who live closer to the equator are less likely to develop MS. The theory is that living closer to the equator results in more sunlight (and thus vitamin D exposure) year-round. Vitamin D is essential for overall immune health.
Smoking
Researchers have been looking at the role of cigarette smoking and higher risk of MS for years. Smoking before the onset of the disease seems to increase the risk significantly. A meta-analysis showed a 1.2 to 1.5-fold increase in the risk of disease.
We do not yet know which pathological changes triggered by smoking influence the development and progression of MS.
Obesity
Being extremely overweight in childhood seems to be a factor in the development of multiple sclerosis in adulthood.
Microbiome
Various studies have shown that the microbiome influences the immune system and autoimmune diseases in general. Intestinal bacteria can dampen or activate the immune.
Epidemiology
According to a study funded by the National MS Society in 2019, nearly 1 million people live with MS in the United States and 2.5 million worldwide. Doctors diagnose most people with MS between the ages of 20 and 50, although it can occur in young children and older adults. While cases of MS are found in most ethnicities, MS is more common in Caucasians of northern European ancestry.
Women are 2 to 3 times more likely to develop MS than men. We also know that MS occurs more frequently in areas that are farther from the equator.
Characteristics and Symptoms
MS signs and symptoms are widely varied among individuals, in both type and amount. Some of the more and less common primary symptoms include:
Common symptoms
- Fatigue
- Walking (gait) difficulties
- Numbness or tingling
- Spasticity
- Weakness
- Problems with vision, loss, and double vision (diplopia)
- Dizziness and vertigo
- Bladder problems
- Sexual problems
- Bowel problems
- Pain and itching
- Cognitive changes
- Emotional changes
- Depression
Less common symptoms
- Speech problems
- Swallowing problems
- Tremor
- Seizures
- Breathing problems
- Hearing loss
MS has different forms of progression, and relapses are common. Experts define a relapse as the occurrence of new or resurgence of already known clinical symptoms that last longer than 24 hours. To distinguish a recent attack from a previous one, there must be at least 30 days between the two clinical events.
The duration of relapse is usually a few days to a few weeks. Depending on whether the symptoms that have occurred recede completely or only incompletely, one speaks of complete or incomplete remission. So-called pseudo relapses happen in the context of a temperature increase or in conjunction with infections and can temporarily worsen clinical symptoms.
MS progression
The first symptoms usually appear between the ages of 15 and 40. Some patients are also slightly younger. While the relapses usually subside entirely at the beginning of the disease, neurological deficits are increasingly left behind in the later course of the disease after relapses.
At the beginning of the disease, doctors and patients frequently observe visual and sensory disturbances. It is not uncommon for the disease to begin with an isolated symptom.
Which symptom develops in a relapse depends on the respective localization of the active demyelinating focus in the central nervous system. For example, inflammation in the area of the optic nerve fibers causes visual disturbances that can manifest themselves as optical blur or milky haze and can also be accompanied by eye pain.
One means of quantifying patient impairment is the use of the Expanded Disability Status Scale (EDSS). Doctors use this scale to classify the current severity of the patient’s disabilities, with a prior assessment of impairments in seven neurological systems. Looking at the entire course of the disease, it is fatigue, bladder dysfunction, and motor system disorders such as paralysis and spasticity that often have the most significant impact on the lives of those affected.
Diagnosis
Your doctor will perform multiple types of tests to diagnose MS and rule out any other conditions, including medical history, a neurologic exam, magnetic resonance imaging (MRI), spinal fluid analysis, and blood tests to rule out other conditions.
Sometimes, doctors diagnose patients exhibiting MS symptoms with clinically isolated syndrome (CIS). CIS presents the same symptoms but, unlike MS, a CIS episode is a singular event while the latter is a lifelong disease. Patients with either condition will receive the same treatment.
Imaging
The brain and spinal cord images obtained by magnetic resonance imaging (MRI) can be used to visualize inflamed and scarred tissue areas. With the aid of a contrast medium containing gadolinium, such as gadopentetate dimeglumine or gadoteric acid, doctors can detect acute disease foci. Periventricular (around the lateral ventricles) sites of inflammation in the medullary bed of the brain and so-called beam sites are typical of MS.
With MRI examination, doctors can detect both the spatial and temporal dissemination of the inflammatory foci in the brain and spinal cord. The McDonald criteria specify exactly how many sites of inflammation in which region of the CNS must be detectable in order to be able to speak of a positive MRI result concerning spatial dissemination. Doctors rarely make a diagnosis of MS based solely on imaging findings.
Other tests
Lumbar puncture (spinal tap): A lumbar puncture is recommended in cases of suspected disease. In 50% of the patients, there is a slight increase of lymphocytic cells in the cerebrospinal fluid (CSF). A chronic inflammatory process in the central nervous system is detectable in more than 95% of the patients.
Evoked potential tests: These tests record the electrical signals produced by your nervous system in response to stimuli, either visual or electrical. In these tests, you watch a moving visible pattern, or a series of short electrical impulses are applied to nerves in your legs or arms. Thus, electrodes measure how fast the information travels through your nerves.
In most people with relapsing-remitting MS, a diagnosis can be made based on a pattern of symptoms consistent with the disease and confirmed by brain imaging scans, such as MRI.
It can be challenging for others with an unusual pattern of symptoms to distinguish MS from other diseases. In addition to infectious diseases, other chronic inflammatory disorders must also be excluded. Other inflammatory demyelinating diseases (such as neuromyelitis optica, tropical spastic paraparesis, or acute disseminated encephalomyelitis (ADEM)) must also be considered. Conditions of the metabolism or a vitamin B12 deficiency can also lead to similar symptoms as in MS.
Treatment
According to the Mayo Clinic, there is no cure for MS. All therapeutic measures aim to slow progression and maintain the patient’s independence in everyday life. This takes the form of increasing recovery times from attacks, slowing the disease progression, and managing MS symptoms.
To treat attacks, patients can use prescription corticosteroids to reduce nerve inflammation, or they can elect to undergo plasma exchange, by which blood is removed from the body, modified, and reinjected.
For primary-progressive MS, ocrelizumab (Ocrevus) is the only medication approved by the U.S. Food and Drug Administration (FDA) as a disease-modifying therapy. Those who receive this treatment are slightly less likely to progress than those who are untreated.
More options are available for persons with relapsing-remitting MS. Since much of the immune response occurs at the start of the disease, early and aggressive treatment with these therapies is associated with better outcomes and longer life expectancy.
Injectable treatments that can alter the immune system’s attacks include interferon beta medications and glatiramer acetate (Copaxone, Glatopa).
There are many oral and infusion treatments available:
Oral:
- Fingolimod (Gilenya)
- Dimethyl fumarate (Tecfidera)
- Diroximel fumarate (Vumerity)
- Teriflunomide (Aubagio)
- Siponimod (Mayzent)
- Cladribine (Mavenclad)
Infusion:
- Ocrelizumab (Ocrevus)
- Natalizumab (Tysabri)
- Alemtuzumab (Campath, Lemtrada)
Besides medication, other strategies may be recommended to help alleviate symptoms, especially with muscle and coordination challenges.
- Physical therapy
- Occupational therapy
- Muscle relaxants
- Medications to reduce fatigue
- Drugs to increase walking speed
- Other medications for conditions such as depression, pain, and bladder control that are often associated with MS
Did you like this article? You can find more posts like this in the Nebula Research Library, including those on other autoimmune disorders such as Addison’s disease, rheumatoid arthritis, lupus, and psoriasis.
June 21, 2022
