精神障害に関する星雲ゲノミクスDNAレポート
精神疾患は遺伝的ですか? この質問に答えようとした研究に基づいて、DNAレポートを作成しました。 以下にサンプルDNAレポートを示します。 パーソナライズされたDNAレポートを入手するには、全ゲノムシーケンス!
で他のレポートを探す星雲図書館:
- (Kunkle 2019) -アルツハイマー病は遺伝的ですか?
- (Dumitrescu 2020) -アルツハイマー病は遺伝的ですか?
- (デミング2019) -認知症は遺伝的ですか?
- (パワー2017) -うつ病は遺伝的ですか?
追加情報
精神障害とは何ですか? (精神疾患は遺伝的ですか?のパート1)
精神疾患または精神障害には、脳と外向きの行動に影響を与える状態が含まれます。 それらは気分障害とも呼ばれます。 精神疾患は、知覚、思考、感情、さらには自己認識の逸脱を伴う可能性があります。 精神疾患は、多くの場合、日常生活のいくつかの領域で機能する重大な個人的な苦痛やストレスや問題につながります。
これらの障害の本質的な要素は、しばしば自分自身を調節する能力の低下です。 この場合、影響を受けた人は、努力、自己規律、または意志力を高めても、病気にほとんどまたはまったく影響を与えることができません。 結果には、日常生活への対処における問題や社会的関係の障害が含まれます。
ザ・世界保健機構世界中で約3億人がうつ病に、4,750万人が認知症に、2,100万人が統合失調症に罹患していると推定されています。 その他のメンタルヘルス障害には、解離性障害、物質使用障害、摂食障害、人格障害が含まれます。 自閉症スペクトラム障害のある人の特定の症状は、精神疾患の症状と似ているように見える場合があります(例、不安神経症やうつ病)。
うつ病は、世界で最も一般的な精神疾患の1つです。
によるアメリカ精神医学会、うつ病の典型的な症状は、気分の落ち込み、陰気、絶望感、ドライブの低下です。 多くの場合、喜びと喜び、自尊心、パフォーマンス、共感、人生への関心が失われます。 その結果、生活の質が損なわれることがよくあります。 これらの苦情は、喪失体験後の悲嘆の文脈で健康な人々に発生し、うつ病として現れます。ただし、通常は自分で通り過ぎます。 症状が不均衡な期間持続する場合、または症状の重症度と期間が不均衡である場合、病気が存在します。
精神医学では、うつ病は情動障害に割り当てられます。 診断は、症状と経過に応じて行われます(例:単一または反復性のうつ病エピソード)。 うつ病の標準的な治療には、個人の固有のニーズに応じて、心理療法と抗うつ薬の使用が含まれます。
医学的には、うつ病は治療を必要とする深刻な精神疾患および病状であり、多くの場合、影響を受ける人の意志力または自己規律によって影響を受けることができない多くの結果をもたらします。 うつ病は主要なメンタルヘルスの危機であり、仕事ができない、または早期退職の主な原因であり、自殺の主な原因です。
疫学(精神疾患は遺伝的ですか?)
国際比較で調査2011年には、高所得国の頻度を中低所得国の頻度と比較しました。 うつ病の生涯有病率は、最初のグループ(10か国)で14.9%、2番目のグループ(8か国)で11.1%でした。 女性と男性の比率は約2:1でした。 による国立精神衛生研究所、米国では推定1,730万人の成人(全米国成人の7.1%)が2017年に少なくとも1つの大うつ病エピソードを発症しました。
米国では、うつ病は人口のほぼ7%に影響を及ぼします。 発症年齢は平均31歳です。
近年、仕事ができなくなったり、入院治療を受けたり、早期退職したりする高齢者など、うつ病による病気の負担が急増しています。 病気の実際の発生率はそれほど深刻に変化しておらず、発生率の増加は精神障害のある人々の認識の向上と汚名の減少によるものと考えられています。 一方、長期的な研究の結果は、実際の増加を示す傾向があり、これはさまざまな社会的影響要因に関連しています。
症状(精神疾患は遺伝的ですか?のパート3)
うつ病の精神疾患の主な症状は次のとおりです。
- うつ病、うつ病の気分:うつ病は、気分の狭まり、または重度のうつ病の場合は「しびれ感」または持続的な内面の空虚感を特徴とします。
- 興味と喜びの喪失:喜びや悲しみを感じる能力の喪失。感情的な共鳴の喪失、すなわち患者の気分は励ましによって明るくすることはできません
- 意欲の欠如と倦怠感の増加:もう1つの典型的な症状は、意欲の抑制です。 重度のうつ病エピソードでは、影響を受けた人々はドライブがひどく抑制され、個人の衛生状態、買い物、洗い物などの最も単純な活動でさえ実行できなくなります。
その他の症状は次のとおりです。
- 集中力と注意力の低下
- 自尊心と自信の低下(不十分感)
- 罪悪感と劣等感
- 否定的で悲観的な将来の見通し(絶望的):特徴は、将来についての誇張された懸念であり、おそらく自分の体の領域の小さな障害(心気症を参照)による誇張された不安、絶望感、無力感、または実際の無力感です
- 自殺念慮または行動:深刻な影響を受けた人は、自分の人生が完全に無意味であると感じることがよくあります。 多くの場合、この苦痛を伴う状態は、潜在的または急性の自殺傾向につながります。
- 不眠症
- 食欲不振
うつ病の人は、しばしば身体的症状、体の非常に異なる部分の痛みを経験します。最も一般的には、胸に苦痛を伴う圧迫感があります。 うつ病エピソードの間、感染症への感受性が高まります。 社会的撤退も観察され、思考が遅くなり(思考の抑制)、無意味な思考の循環(ひなへの衝動)、時間感覚の乱れが見られます。 過敏性と不安がしばしば存在します。 さらに、ノイズに対する過敏症が問題になる可能性があります。 双極性障害もうつ病のサブグループであり、患者が重度の躁病の発作を経験し、その後、うつ病や不安神経症が長引くと発生します。 うつ病は不安障害でも発生する可能性があります。
重大度
重症度(精神疾患は遺伝的ですか?のパート3.1)は、症状の数に応じて分類されます。
- 軽度のうつ病:2つの主な症状と2つの追加の症状
- 中等度のうつ病:2つの主な症状と3〜4つの追加の症状
- 重度のうつ病:3つの主な症状と5つ以上の追加の症状
性差
うつ病の症状は、性別によってさまざまな形で現れる可能性があります。 主要な症状の違いはわずかです。 女性では、落胆や陰気などの現象がより一般的ですが、男性では、うつ病が積極的に行動する傾向にも反映されている可能性があるという明確な証拠があります。 2014年に調査、女性と男性の異なる症状は、ストレス反応の生物学的システムの違いに関連していました。
:max_bytes(150000):strip_icc()/common-types-of-depression-1067313_V4-85226c22cdbc4083a9d4c6e0b21f2a80.png)
原因(精神疾患は遺伝的ですか?のパート4)
精神疾患やうつ病の原因は複雑で、部分的にしか理解されていません。 精神疾患の発症には、素因と後天的な感受性の両方があります。 後天的な感受性は、生物学的要因および生活史上の社会的または心理的ストレスによって引き起こされる可能性があります。 季節性情動障害は、季節の変化と相関する特定のタイプのうつ病でもあります。

うつ病は遺伝的ですか? (精神疾患は遺伝的ですか?のパート5)
うつ病は家族で起こる可能性がありますが、双生児研究では、遺伝的要素が障害に寄与する唯一の要因であることが示されました。 同一の遺伝子構成(同一の双子)であっても、うつ病の兄弟を持つ人は、症例の半分未満で精神疾患を発症する傾向があります。 影響を受けた双子のパートナーと影響を受けていない双子のパートナーの違いは、遺伝情報のその後の(エピジェネティックな)変化、つまり遺伝情報の制御に対する生活史の影響にも見られます。 これは、うつ病の両親や兄弟にも影響を及ぼしています。 いずれにせよ、完全な家族歴は、うつ病の家族を見つけるために、各患者の症例の遺伝的根拠に対処するのに役立ちます。 しかし、影響を受けた親戚がうつ病や他の精神疾患の症状を決して発症しない可能性があります。
さらに、遺伝的要因と環境要因の間には遺伝子と環境の相互作用があり、うつ病を発症する人々に影響を与えます。 たとえば、遺伝的要因により、特定の人は、リスクを冒そうとする意欲を持って、困難な生活状況に陥ることがよくあります。 逆に、人が心理社会的負担に対処するか、うつ病になるかは、遺伝的要因に依存する可能性があります。
うつ病の発生の重要な遺伝的脆弱性要因は、セロトニントランスポーター遺伝子5-HTTLPRのプロモーター領域の変異であると疑われています。 5-HTTLPRは、セロトニン(5-HT)トランスポーター(T)長さ(L)多型(P)領域(R)の略です。 この「うつ病遺伝子」は染色体17q11.1-q12に位置し、集団内でさまざまな形態で発生します(「短い」対立遺伝子と「長い対立遺伝子」を伴ういわゆる「異なる長さの多型」)。 短い対立遺伝子の保因者は心理社会的ストレスに対してより敏感に反応し、長い対立遺伝子の保因者よりもうつ病を発症するリスク(気質)が最大2倍あると言われています。
の2つのメタアナリシスで2011 、ストレス後の短い対立遺伝子とうつ病の発症との関連が確認されました。 のメタアナリシスで2014年、5HTTP / SLC6A4、APOE、DRD4、GNB3、HTR1A、MTHFR、およびSLC6A3の合計7つの候補遺伝子のうつ病に関連して有意なデータが見つかりました。 しかし、非常に広範囲にわたる調査にもかかわらず、うつ病の発症を決定する特定の異常はまだ発見されていません。
うつ病を発症する危険因子には、心的外傷、他の精神疾患の病歴、特定の薬の服用、重篤または慢性の病気の経験が含まれます。
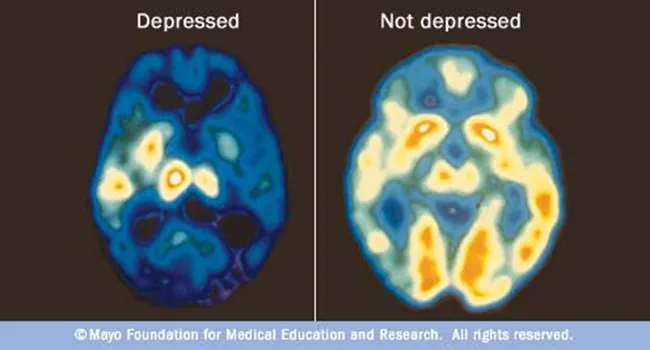
神経生理学
1950年代にレセルピンが薬として導入された後、レセルピンで治療された後に精神疾患の症状を示す患者が観察されました。 これは、脳内の神経伝達物質の低下に起因していました。 信号伝達が特にモノアミン作動性神経伝達物質であるセロトニン、ドーパミン、ノルアドレナリンに関与していることは確かであると考えられています。 他の信号システムも関与しており、それらの相互影響は非常に複雑です。 モノアミン作動性の影響薬(抗うつ薬)はうつ病の症状を変える可能性がありますが、これらの伝達システムがうつ病の発症にどの程度因果関係があるのかは不明です。 したがって、患者の約3分の1は、モノアミン作動系に影響を与える薬剤に反応しないか、反応が不十分です。
治療(精神疾患は遺伝的ですか?のパート6)
うつ病は、大多数の患者でうまく治療することができます。 可能な治療オプションには、抗うつ薬による薬物治療、心理療法、または薬物と心理療法の組み合わせが含まれます。 これは、オンライン療法プログラムによってますます補完され、サポートされています。 光線療法または睡眠療法、スポーツおよび運動療法などの持続性抑うつ障害の他の治療法は、治療オプションを補完します。
現在の国内治療ガイドラインでは、抗うつ薬は中等度から重度のうつ病期間の心理療法と同等であると見なされています。 重度のうつ病には、心理療法と抗うつ薬の併用が推奨されます。 最終的に、精神疾患を治療するためのアプローチは、ケースバイケースで医療専門家によって処理されます。
心理療法と薬物治療の組み合わせは、心理療法の訓練を受けた医師またはメンタルヘルスの専門家によって、あるいは外来で、または精神科の診療所や専門病院で医師と心理療法士の協力によって行うことができます。
外来治療や向精神薬に対する苦痛が大きく、反応が不十分な場合、特に自殺が差し迫っている場合は、精神科クリニックでの治療を検討する必要があります。
うつ病やその他のメンタルヘルスの問題を抱えている人は、通常、心臓病などの他の慢性的な問題のリスクも高くなります。
精神疾患に苦しむ人々のために、一般の人々が無料で利用できる複数のホットラインが存在します。 たとえば、薬物乱用およびメンタルヘルスサービスの管理部門は、精神に直面している個人および家族向けに、24時間年中無休の無料の機密の治療紹介および情報サービス(英語およびスペイン語)である全国ヘルプラインを提供しています。および/または物質使用障害。
自殺を感じた場合は、すぐに911または最寄りの緊急電話番号に電話してください。 National Suicide Prevention Lifelineには、1-800-273-TALK(1-800-273-8255)でアクセスできます。
薬物(精神疾患は遺伝的ですか?のパート6.1)
抗うつ薬
うつ病では、あるニューロンの軸索(上)から別のニューロンの樹状突起(下)への信号伝達が増加します。たとえば、放出された神経伝達物質を軸索に戻すトランスポーターをブロックすることによってです。 これにより、細胞間のシナプス間隙内の伝達物質の量が増加し、細胞から細胞への信号伝達が増加します。 このようなトランスポーターをブロックする薬は、抗うつ薬に典型的です。
精神疾患を治療するための抗うつ薬の有効性は、精神疾患の重症度に強く依存しています。 軽度および中等度の重症度では有効性がないか低いですが、重度のうつ病ではより高くなります。 最も重症の場合、治療を受けた患者の最大30%が抗うつ薬の恩恵を受けます。 メタ研究は、抗うつ薬が患者ごとにその有効性に大きな違いを示すことを示しています。 場合によっては、異なる薬の組み合わせが利点を持つことができます。
選択的再取り込み阻害剤
これらの有効成分は、神経伝達物質であるセロトニン、ノルエピネフリン、またはドーパミンのシナプス前部への再取り込みを阻害します。 他の神経伝達物質への直接的な影響は、これらの選択的薬剤の方が三環系抗うつ薬よりも著しく弱いです。
選択的セロトニン再取り込み阻害薬(SSRI)は、今日のうつ病に最も一般的に使用されている薬です。 それらは2から3週間の期間有効です。 それらは(大部分)シナプス前膜でのセロトニンの再取り込みを選択的に阻害します。 これは、信号伝達中にメッセンジャー物質セロトニンの「相対的な」増加をもたらします。
モノアミノオキシダーゼ(MAO)阻害剤
MAO阻害剤は、モノアミンオキシダーゼ酵素をブロックすることによって機能します。 これらの酵素は、セロトニン、ノルエピネフリン、ドーパミンなどのモノアミンを切断します。 これにより、脳内での信号伝達の可用性が低下します。 MAO阻害剤はこれらの酵素を阻害し、モノアミンの濃度を高め、神経伝達物質の濃度を高めます。 これにより、神経細胞間の信号伝達が強化されます。
MAO阻害剤は、選択的または非選択的と可逆的または不可逆的に分類されます。 MAO-Aの選択的阻害剤(例、モクロベミド、可逆性)は、A型モノアミンオキシダーゼのみを阻害し、抗うつ効果を示します。 それらは、SSRIよりも消化機能および性機能の障害が大幅に少ないことを含め、一般的に忍容性が良好です。
ケタミン
うつ病の緊急事態(自殺のリスク)では、いくつかの研究でケタミンの急速な抗うつ効果が確認されました。 これは、グルタメートNMDA受容体複合体の拮抗薬です。 研究結果は、一度投与された場合、最大7日間の期間にわたって有意な改善を示しました。 低用量処方のための推奨事項があります。 麻酔薬や解離薬として使用するのとは対照的に、副作用はほとんどありません。
メンタルヘルス状態のある人のための代替アプローチ
- 光線療法
- 運動
- 栄養
- 睡眠モニタリング
- 睡眠不足
- 瞑想
- サポートグループ
この記事は楽しかったですか? 私たちのこのような記事をもっと読む星雲研究図書館!抗うつ薬のような薬のレビューにも興味があるかもしれませんLexaproそしてゾロフト。
